 Interventions related to central venous catheters were, on average, associated with 57% fewer bloodstream infections and substantial savings to hospitals, found a multi-centre analysis.
Interventions related to central venous catheters were, on average, associated with 57% fewer bloodstream infections and substantial savings to hospitals, found a multi-centre analysis.
US hospitals are reducing bloodstream infections related to catheters by implementing rigorous safeguards that also save millions of healthcare dollars each year, according to research led by Cedars-Sinai. "Safety interventions are a win-win for both patients and hospitals," said Dr Teryl Nuckols, director of the division of general internal medicine in the Cedars-Sinai department of medicine.
Nuckols led a multi-centre team that studied data published in the last decade on catheter-related bloodstream infections at 113 hospitals. The team found that safety interventions, on average, reduced the infection rate by 57% at these hospitals while producing net savings of $1.85m for each site over three years. The savings came from reduced costs in treating infected patients.
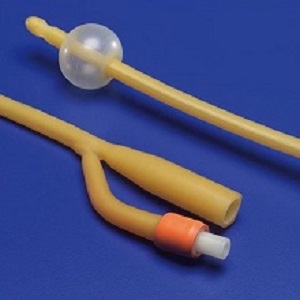
The study focused on central venous catheters, also known as central lines, which are commonly used in intensive care units. These lines are placed in large veins in the arm, chest, neck or groin to deliver medications, fluids or blood to patients.
More than 60,000 primary bloodstream infections related to these catheters are estimated to occur each year in the US, with a fatality rate of 12% or more, according to recent studies. To prevent these infections, hospitals in recent years have introduced new safety procedures. Checklists for attending staff include donning sterile gloves, covering catheters with antimicrobial dressings and checking catheters daily for signs of movement or infection. Many hospitals also have invested in extra training, equipment and supplies to improve safety.
The phasing-in of these safeguards correlated with a 49% reduction nationally in the rate of catheter-related bloodstream infections from 2010 to 2013, according to the federal Agency for Healthcare Research and Quality. The new Cedars-Sinai-led study shows that these safeguards, while adding to equipment and labour costs, ultimately reduced infections and saved money.
In the hospitals studied, the median cost of implementing catheter safety programmes was about $270,000 per site. But for every $100,000 that a hospital spent, it realised an average $315,000 savings because it treated fewer infected patients, the investigators found. Although savings were lower in certain hospitals that already had low infection rates, adding new precautions still paid off for them.
Nuckols said the study supports the value of medical centers upgrading their safety procedures to prevent catheter infections. "Due to the high cost of caring for patients when central-line infections develop, even sizable up-front investments in infection prevention can be associated with large net savings," Nuckols said. "On the basis of our findings, hospitals that have not yet achieved very low rates of infection can consider implementing a variety of safety practices."
Abstract
Importance: Although quality improvement (QI) interventions can reduce central–line-associated bloodstream infections (CLABSI) and catheter-related bloodstream infections (CRBSI), their economic value is uncertain.
Objective: To systematically review economic evaluations of QI interventions designed to prevent CLABSI and/or CRBSI in acute care hospitals.
Evidence Review: A search of Ovid MEDLINE, Econlit, Centre for Reviews & Dissemination, New York Academy of Medicine's Grey Literature Report, Worldcat, prior systematic reviews (January 2004 to July 2016), and IDWeek conference abstracts (2013-2016), was conducted from 2013 to 2016. We included English-language studies of any design that evaluated organizational or structural changes to prevent CLABSI or CRBSI, and reported program and infection-related costs. Dual reviewers assessed study design, effectiveness, costs, and study quality. For each eligible study, we performed a cost-consequences analysis from the hospital perspective, estimating the incidence rate ratio (IRR) and incremental net savings. Unadjusted weighted regression analyses tested predictors of these measures, weighted by catheter-days per study per year.
Findings: Of 505 articles, 15 unique studies were eligible, together representing data from 113 hospitals. Thirteen studies compared Agency for Healthcare Research and Quality–recommended practices with usual care, including 7 testing insertion checklists. Eleven studies were based on uncontrolled before-after designs, 1 on a randomized controlled trial, 1 on a time-series analysis, and 2 on modeled estimates. Overall, the weighted mean IRR was 0.43 (95% CI, 0.35-0.51) and incremental net savings were $1.85 million (95% CI, $1.30 million to $2.40 million) per hospital over 3 years (2015 US dollars). Each $100 000-increase in program cost was associated with $315 000 greater savings (95% CI, $166 000-$464 000; P < .001). Infections and net costs declined when hospitals already used checklists or had baseline infection rates of 1.7 to 3.7 per 1000 catheter-days. Study quality was not associated with effectiveness or costs.
Conclusions and Relevance: Interventions related to central venous catheters were, on average, associated with 57% fewer bloodstream infections and substantial savings to hospitals. Larger initial investments may be associated with greater savings. Although checklists are now widely used and infections have started to decline, additional improvements and savings can occur at hospitals that have not yet attained very low infection rates.
Authors
Teryl K Nuckols, Emmett Keeler, Sally C Morton, Laura Anderson, Brian Doyle, Marika Booth, Roberta Shanman, Jonathan Grein, Paul Shekelle
[link url="https://www.sciencedaily.com/releases/2017/01/170109102650.htm"]Cedars-Sinai material[/link]
[link url="http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2571616"]JAMA Internal Medicine abstract[/link]
