 After screening 15,000 women over a period of five years, a major clinical study in Sweden has shown that 3D mammography, or breast tomosynthesis, detects over 30% more cancers compared to traditional mammography – with a majority of the detected tumours proving to be invasive cancers. The extensive screening study was conducted by Lund University and Skåne University Hospital in Sweden.
After screening 15,000 women over a period of five years, a major clinical study in Sweden has shown that 3D mammography, or breast tomosynthesis, detects over 30% more cancers compared to traditional mammography – with a majority of the detected tumours proving to be invasive cancers. The extensive screening study was conducted by Lund University and Skåne University Hospital in Sweden.
"With breast tomosynthesis, 34% more cancer tumours were detected compared to the current standard mammography screening. At the same time, we were able to reduce the compression of the breast during examination, something that may encourage more women to participate in screening," explains Sophia Zackrisson, associate professor at Lund University and radiologist at Skåne University Hospital (SUS). "We did, however, need to call back a few more women for additional examinations compared to traditional mammography. We needed to confirm that these women did not have cancer, as this method finds more structures in the breast in general. So, there was an increased call-back rate."
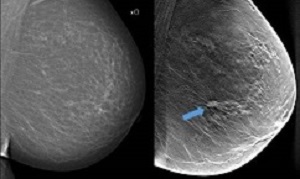
In traditional mammography screening, all breast tissue is captured in a single image. Breast tomosynthesis, on the other hand, is three-dimensional and works according to the same principle as what is known as tomography. This means that several low-dose x-ray images are taken of the breast from different angles, which are reconstructed by a computer to show thin layers of the breast. With more and improved image information and less overlapping tissue structures, the chance of detecting tumours increases.
Further, the radiation dose may be lowered in certain circumstances. "There is a need to improve screening for many women, and breast tomosynthesis is clearly the most appropriate method to transition to in breast cancer screening. Breast tomosynthesis will be introduced, it's just a question of when and to what extent," says Zackrisson.
Breast tomosynthesis is already used at Skåne University Hospital, among other places, to investigate suspected breast cancer. Prior to a possible large-scale introduction in the general breast cancer screening programme, the research team is now conducting a cost-benefit study.
All types of screening involve a risk of overdiagnosis, which in turn may lead to unjustified treatments. Therefore, the research team, in collaboration with their European colleagues, will conduct a meta-study in which they will aggregate and analyse their collective research results.
The lack of radiologists who can review the increased image material generated by 3D methods presents a further challenge before large-scale introduction. However, the method used at Skåne University Hospital may be more efficient than those previously examined in international studies. In Skåne, only the 3D method has been used whereas other studies have combined 3D with traditional mammography screening. This leads to more image material and a higher radiation dose.
"We have shown that we can achieve the same result with a simpler and perhaps even better method," says Zackrisson.
In the future, parts of the image review in connection with breast tomosynthesis may be automated with the help of computers, but it will take time. There is currently a lack of appropriate ready-to-use and tested software. Studies are underway, including in Zackrisson's research team.
Summary
Background: Digital breast tomosynthesis is an advancement of the mammographic technique, with the potential to increase detection of lesions during breast cancer screening. The main aim of the Malmö Breast Tomosynthesis Screening Trial (MBTST) was to investigate the accuracy of one-view digital breast tomosynthesis in population screening compared with standard two-view digital mammography.
Methods: In this prospective, population-based screening study, of women aged 40–74 years invited to attend national breast cancer screening at Skåne University Hospital, Malmö, Sweden, a random sample was asked to participate in the trial (every third woman who was invited to attend regular screening was invited to participate). Participants had to be able to speak English or Swedish and were excluded from the study if they were pregnant. Participants underwent screening with two-view digital mammography (ie, craniocaudal and mediolateral oblique views) followed by one-view digital breast tomosynthesis with reduced compression in the mediolateral oblique view (with a wide tomosynthesis angle of 50°) at one screening visit. Images were read with masked double reading and scoring by two separate reading groups, one for each method, made up of seven radiologists. Any cancer detected with a malignancy probability score of three or higher by any reader in either group was discussed in a consensus meeting of at least two readers, from which the decision of whether or not to recall the woman for further investigation was made. The primary outcome measures were sensitivity and specificity of breast cancer detection. Secondary outcome measures were screening performance measures of cancer detection, recall, and interval cancers (cancers clinically detected between screenings), and positive predictive value for screen recalls and negative predictive value of each method. Outcomes were analysed in the per-protocol population. Follow-up of the participants for at least 2 years allowed for identification of interval cancers. This trial is registered with ClinicalTrials.gov, number NCT01091545.
Findings: Between Jan 27, 2010, and Feb 13, 2015, of 21 691 women invited, 14 851 (68%) agreed to participate. Three women withdrew consent during follow-up and were excluded from the analyses. 139 breast cancers were detected in 137 (<1%) of 14 848 women. Sensitivity was higher for digital breast tomosynthesis than for digital mammography (81·1%, 95% CI 74·2–86·9, vs 60·4%, 52·3–68·0) and specificity was slightly lower for digital breast tomosynthesis than was for digital mammography (97·2%, 95% CI 97·0–97·5, vs 98·1%, 97·9–98·3). The proportion of cancers detected was significantly higher with digital breast tomosynthesis than with digital mammography (8·7 cancers per 1000 women screened, 95% CI 7·3–10·3 vs 6·5 cancers per 1000 screened, 5·2–7·9; p<0·0001). The proportion of women recalled after discussion was higher among cancers detected by digital breast tomosynthesis than for those detected by digital mammography after consensus (3·6%, 95% CI 3·3–3·9 vs 2·5%, 2·2–2·8; p<0·0001). The positive predictive value for screen recalls was 24·1% (95% CI 20·5–28·0) for digital breast tomosynthesis and 25·9% (21·6–30·7) for digital mammography, and the negative predictive value was 99·8% (99·7–99·9) and 99·6% (99·4–99·7), respectively. The proportion of women who developed interval cancers after trial screening was 1·48 cancers per 1000 women screened (95% CI 0·93–2·24).
Interpretation: Breast cancer screening by use of one-view digital breast tomosynthesis with a reduced compression force has higher sensitivity at a slightly lower specificity for breast cancer detection compared with two-view digital mammography and has the potential to reduce the radiation dose and screen-reading burden required by two-view digital breast tomosynthesis with two-view digital mammography.
Authors
Sophia Zackrisson, Kristina Lång, Aldana Rosso, Kristin Johnson, Magnus Dustler, Daniel Förnvik, Hannie Förnvik, Hanna Sartor, Pontus Timberg, Anders Tingberg, Ingvar Andersson
[link url="https://www.lunduniversity.lu.se/article/3d-mammography-detected-34-more-breast-cancers-in-screening"]Lund University material[/link]
[link url="https://www.sciencedirect.com/science/article/pii/S1470204518305217?via%3Dihub"]The Lancet Oncology article summary[/link]
