A patient in their 40s had presented with complaints of intermittent episodes of palpitations for the past year.
The patient described the palpitations as sudden in onset, persisting for two to three minutes, and terminating spontaneously and abruptly. The frequency of these palpitation episodes varied from once per week to less than once per month.
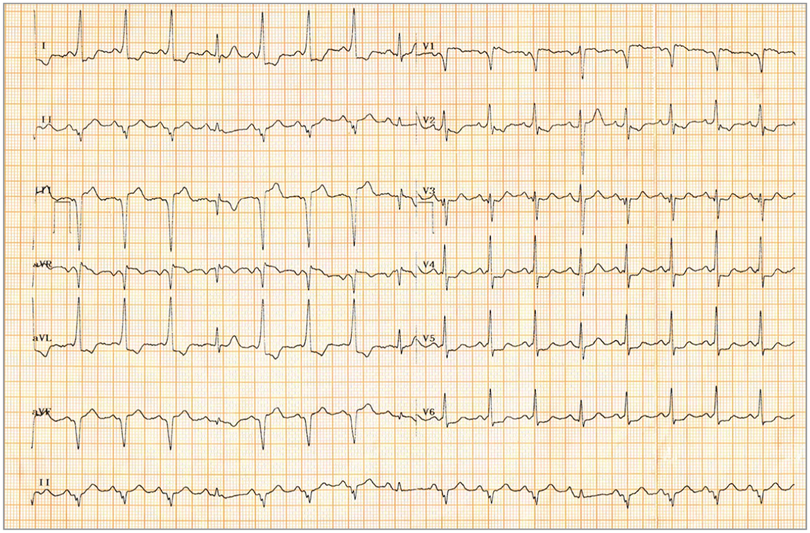
There were no associated syncopal episodes or giddiness. All of the episodes terminated before the patient could reach the hospital,write Drs Ramanathan Velayutham, Chinmay Parale and Dinakar Bootla, from the Jawaharlal Institute of Postgraduate Medical Education and Research in Puducherry, India in JAMA Internal Medicine. There was no other contributory history. At presentation, the patient was in sinus rhythm with pulse rate of 100 beats/min, blood pressure of 126/80 mm Hg, and a normal cardiovascular examination.
Questions: What is the likely location of the accessory pathway? Does this accessory pathway need radio-frequency ablation?
Interpretation
The ECG showed intermittent pre-excitation; pre-excited beats had a short PR interval (90 milliseconds), a QRS duration of 100 milliseconds, and discordant ST-segment and T-wave changes. Delta waves were negative in leads V, III, and aVF and positive in leads V, I, and aVL, suggestive of a posteroseptal pathway. Intermittent pre-excitation on the surface ECG is classically thought to correlate with slower ventricular rates during atrial fibrillation compared with patients with persistent pre-excitation; this is due to longer accessory pathway effective refractory periods (APERPs) in patients with intermittent pre-excitation. Because the chances of degeneration into ventricular fibrillation are smaller at lower ventricular rates, intermittent pre-excitation indicates an accessory pathway at a low risk for sudden cardiac death.
Clinical course
Transthoracic echocardiography demonstrated a structurally normal heart with normal left ventricular systolic function. Because of recurrent symptoms, the patient was advised to undergo an electrophysiological study to look for high-risk characteristics, despite the surface ECG suggesting otherwise.
Electrophysiological study results revealed the presence of a posteroseptal accessory pathway with an effective refractory period of 240 milliseconds. Tachycardia could be successfully induced with a single atrial extrastimulus, and the tachycardia rate was 220 beats/min.
Considering the presence of recurrent palpitation episodes, a short APERP, and tachycardia inducibility with atrial extrastimulus testing, the accessory pathway was deemed to be high risk and was successfully ablated. The postablation ECG showed absence of delta waves.
Discussion
Various algorithms have been established for localising the accessory pathways based on the surface ECG. The most widely studied and well-established Arruda algorithm suggested the presence of a posteroseptal accessory pathway in this patient. Risk stratification of accessory pathways depends on the identification of markers for sudden cardiac death. These include smaller APERP (less than 250 milliseconds), shortest pre-excited R-R intervals of less than 250 milliseconds during atrial fibrillation, presence of multiple accessory pathways, Ebstein anomaly, and familial Wolff-Parkinson-White (WPW) syndrome.
On the other hand, abrupt loss of pre-excitation during treadmill testing and intermittent pre-excitation on the surface ECG imply the presence of bypass tracts with longer refractory periods.
The coronary sinus pathway is associated with coronary sinus aneurysm, which is found to have a rapid conduction time and thereby high risk of fast ventricular rate and sudden cardiac death during atrial fibrillation episodes.
Multiple studies have shown that intermittent pre-excitation on the surface ECG is associated with pathways that are at a lower risk of ventricular fibrillation and sudden cardiac death. Klein and Gulamhusein studied 52 patients with WPW syndrome, of whom 26 had intermittent loss of pre-excitation on the surface ECG.
It was found that patients with intermittent pre-excitation had longer APERPs and also longer shortest pre-excited R-R intervals during atrial fibrillation compared with patients with persistent pre-excitation, suggesting a low risk of developing fast ventricular rate in the event of atrial fibrillation. Mah et al studied 41 children with intermittent pre-excitation and came to a similar conclusion of longer APERPs in patients with intermittent pre-excitation.
However, the assumption that intermittent pre-excitation on the surface ECG points toward a low-risk pathway is not always true, as was seen in this case. In a study of 56 patients with WPW syndrome and ventricular fibrillation, Orczykowski et al found that four patients had intermittent pre-excitation on the resting ECG. Similarly, Kiger et al, in a study of 295 children with pre-excitation, found that there was no difference in the frequency of high-risk pathways in patients with intermittent pre-excitation compared with those with persistent pre-excitation.
One of the probable explanations for this phenomenon can be a higher catecholamine sensitivity of the accessory pathway in some patients with intermittent pre-excitation. In a case report by Aleong et al, a 50-year-old man with intermittent pre-excitation at baseline was found to have a marked sensitivity to adrenergic stimulation, which was demonstrated by 1:1 pre-excitation at peak exercise and with isoproterenol administration.
A treadmill test could have supported this hypothesis in the current patient but was not performed. Six months after the radiofrequency ablation, the patient was asymptomatic and continued to undergo regular follow-up.
Take-home points
• Risk stratification of an accessory pathway depends on how rapidly it conducts during atrial fibrillation.
• Non-invasive findings that identify low-risk pathways include intermittent loss of pre-excitation on the resting ECG or during ambulatory monitoring and abrupt loss of pre-excitation during exercise testing.
• Symptomatic patients with manifest pre-excitation should undergo an invasive electrophysiological study for risk assessment, even if the non-invasive assessment suggests otherwise.
• All pathways with intermittent pre-excitation on the surface ECG need not be low risk.
See more from MedicalBrief archives:
Prohibitions against caffeine to reduce cardiac arrhythmias ‘unwarranted’ — UK cohort study
58% of sudden cardiac arrest victims had contracted health services before
Heightened risk of AF in congenital heart disease patients
Implanted cardiac monitors successful with undiagnosed AF
SA scientists collaborate in ‘sudden death’ gene mutation discovery
