 A study has found that black women in South Africa are almost six times more likely to die of cervical cancer than white women and that the five-year survival rates of black and coloured women (40-50%) were significantly worse than those of white and Indian women (60-80%).
A study has found that black women in South Africa are almost six times more likely to die of cervical cancer than white women and that the five-year survival rates of black and coloured women (40-50%) were significantly worse than those of white and Indian women (60-80%).
Researchers at the School of Public Health, University of the Witwatersrand, Wits Reproductive Health & HIV Institute, University of the Witwatersrand and the National Cancer Registry, National Health Laboratory Service, Johannesburg, analysed 1994-2009 cervical cancer data from the South African National Cancer Registry and mortality rates from Stats SA. At the time the study began, the data for cancer incidences and mortality were not available later than 2009 and until 2012 respectively.
In 2014, 5,000 black women were diagnosed with cervical cancer in South Africa alone.
The study revealed that about 75,000 cases of cervical cancer were reported between 1994 and 2009, with an average of close to 5,000 each year. Most cases (90%) were diagnosed in government laboratories.
The report says poor screening is one of the reasons cervical cancer is not detected early. “There’s a long turnaround time for results of Pap smears. We also do not have a system in place to call patients back to the clinic for results, so they may not know they have a pre-cancerous lesion or cervical cancer,” explains says Dr Elvira Singh, head of the country’s National Cancer Registry.
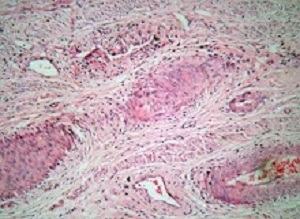
The Human Papilloma Virus – commonly referred to as HPV – is the leading cause of cervical cancer in South Africa, says Singh in the report. HPV is a very common virus that infects most people, but if the infection persists women are at risk of developing cervical cancer. According to the World Health Organisation, HPV is one of the most common sexually transmitted viruses.
There are often no visible symptoms for HPV and it is most likely to infect adolescent girls and young women. “Women who are sexually active acquire an HPV infection and more often than not the immune system takes care of it and the infection goes away. It’s the persistence of HPV infection that drives the cancer burden,” says Singh.
Having a family history of cancer, being overweight and smoking increase the risk of cervical cancer. HIV infection also causes HPV to persist and accelerates the conversion from pre-cancerous lesions to cervical cancer, Singh adds.
South Africa has a high burden of HIV. The latest HIV household survey estimated that there were 231,100 new HIV infections in 2017. Women between the ages of 15 and 24 make up a third of new infections in South Africa. Singh says: “In the HIV-infected population, women develop cervical cancer at a younger age than in the HIV-uninfected population.”
According to the latest figures from the South African National Cancer Registry, there were 5,735 new cases of cervical cancer in the country in 2014. Of those, black women account for 85% of new infections.
“While breast cancer is the number one cancer in white women, cervical cancer is the number one cancer in black women. This is because of the higher rates of HPV infection, HIV as well as the sexual and reproductive risk factors that are different in black women compared with other ethnic groups,” explains Singh in the report.
Vaccination is the number one preventative measure against cervical cancer and the government is rolling out HPV vaccinations at schools. But these must be done before girls and women start having sex, says Singh.
Women can also lower their risk of cervical cancer by consistently using condoms during sex to prevent HPV and HIV infections and screening to detect pre-cancers before they turn into cervical cancer by going for Pap smears.
Abstract
Cervical cancer (CC) is the leading cause of cancer death among female South Africans (SA). Improved access to reproductive health services following multi‐ethnic democracy in 1994, HIV epidemic, and the initiation of CC population‐based screening in early 2000s have influenced the epidemiology of CC in SA. We therefore evaluated the trends in CC age‐standardised incidence (ASIR) (1994–2009) and mortality rates (ASMR) (2004–2012) using data from the South African National Cancer Registry and the Statistics South Africa, respectively. Five‐year relative survival rates and average per cent change (AAPC) stratified by ethnicity and age‐groups was determined. The average annual CC cases and mortalities were 4,694 (75,099 cases/16 years) and 2,789 (25,101 deaths/9 years), respectively. The ASIR was 22.1/100,000 in 1994 and 23.3/100,000 in 2009, with an average annual decline in incidence of 0.9% per annum (AAPC = −0.9%, p‐value < 0.001). The ASMR decreased slightly by 0.6% per annum from 13.9/100,000 in 2004 to 13.1/100,000 in 2012 (AAPC = −0.6%, p‐value < 0.001). In 2012, ASMR was 5.8‐fold higher in Blacks than in Whites. The 5‐year survival rates were higher in Whites and Indians/Asians (60–80%) than in Blacks and Coloureds (40–50%). The incidence rate increased (AAPC range: 1.1–3.1%, p‐value < 0.001) among young women (25–34 years) from 2000 to 2009. Despite interventions, there were minimal changes in overall epidemiology of CC in SA but there were increased CC rates among young women and ethnic disparities in CC burden. A review of the CC national policy and directed CC prevention and treatment are required to positively impact the burden of CC in SA.
Authors
Gbenga Olorunfemi, Ntombizodwa Ndlovu, Gwinyai Masukume, Admire Chikandiwa, Pedro T Pisa, Elvira Singh
[link url="https://www.dailymaverick.co.za/article/2018-11-04-race-determines-survival-in-sas-cervical-cancer-patients/"]Daily Maverick report[/link]
[link url="https://onlinelibrary.wiley.com/doi/pdf/10.1002/ijc.31610"]Cancer Genetics and Epigenetics abstract[/link]
