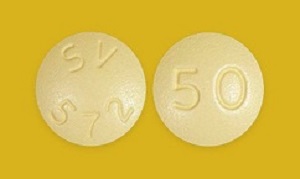
 Data presented at the Conference on Retroviruses and Opportunistic Infections (CROI 2018) in Boston from the 24-week interim analysis of the INSPIRING clinical trial showed that dolutegravir administered at 50mg twice-daily with dual nucleoside reverse transcriptase inhibitors (NRTI), was effective and well-tolerated in HIV/TB co-infected adults receiving rifampin-based TB therapy. The CROI abstract which reported on outcomes of 69 TB patients who were treated with dolutegravir showed viral suppression of <50 c/mL at 24 weeks of 81%. TB associated IRIS at 4% was low, there were no new toxicity signals for dolutegravir and no patients discontinued treatment due to IRIS or liver events.
Data presented at the Conference on Retroviruses and Opportunistic Infections (CROI 2018) in Boston from the 24-week interim analysis of the INSPIRING clinical trial showed that dolutegravir administered at 50mg twice-daily with dual nucleoside reverse transcriptase inhibitors (NRTI), was effective and well-tolerated in HIV/TB co-infected adults receiving rifampin-based TB therapy. The CROI abstract which reported on outcomes of 69 TB patients who were treated with dolutegravir showed viral suppression of <50 c/mL at 24 weeks of 81%. TB associated IRIS at 4% was low, there were no new toxicity signals for dolutegravir and no patients discontinued treatment due to IRIS or liver events.
John C Pottage, chief scientific and medical officer, ViiV Healthcare notes that, “… Concurrent treatment of TB and HIV remains a challenge as it is compounded by drug interactions, overlapping toxicities and immune reconstitution inflammatory syndrome… The INSPIRING results add to the breadth and depth of data available for dolutegravir and support its use in the treatment of people living with HIV co-infected with TB.”
The early results of this study are encouraging as dolutegravir is increasingly being prescribed as a first line treatment option with little evidence on acceptability of use and dosage in patients co-infected with TB. Considering the recent reports of the termination of a dolutegravir PK study with weekly rifapentine and INH due to serious toxicity, the INSPIRING study provides conflicting evidence of dolutegravir safety with TB treatment. The authors of the PK study which was also presented at CROI noted that the two patients who exhibited toxicity both had high INH levels but could not determine the cause of the toxicity.
In a commentary on healio.com, Dr Richard Kaplan and Professor Robin Wood from the Desmond Tutu HIV Foundation note that the PK study highlights a potential for dolutegravir interaction with rifamycin TB drugs and refer to a previous small PK study of dolutegravir with either rifampicin or rifabutin, which reported one serious adverse event attributed to rifamycin hypersensitivity syndrome among 27 healthy volunteers. They also note that rifapentine has also been shown to cause a not insubstantial number of systemic drug reactions in a previous study which occurred more frequently in participants receiving concomitant non-study medication.
That similar toxicities have not been reported in the INSPIRING study is encouraging for the potential use of dolutegravir at the 50mg twice daily regimen with standardised daily TB treatment. Also considering the concern that rapid onset of virological suppression induced by dolutegravir could result in increased TB IRIS, the low IRIS rates on the INSPIRING study and the absence of treatment discontinuations due to IRIS is a very positive finding. However, the median baseline CD4 count of patients on the INSPIRING study was reported as 208 cells/µL which is relatively high. IRIS rates may be higher and more severe in patients at lower CD4 counts.
The INSPIRING study is ongoing and is yet to report on the final week 48 TB and HIV treatment outcomes data.
Abstract 1
Concurrent treatment of TB and HIV is compounded by drug interactions, overlapping toxicities, and immune reconstitution inflammatory syndrome (IRIS). The efficacy and safety of dolutegravir (DTG) in antiretroviral treatment (ART) naïve adults with HIV/TB co-infection was assessed.
INSPIRING (NCT02178592) is a Phase 3b, non-comparative, active control, randomised, open-label study in HIV-1 infected ART-naïve adults (CD4+ ≥50 cells/µL) with drug-sensitive TB. Participants on rifampin-based TB treatment for up to 8 weeks were randomised (3:2) to receive DTG (50mg twice daily during and for 2 weeks post-TB therapy, followed by 50mg once daily [OD]) or EFV (600mg OD), with 2 investigator-selected NRTIs for 52 weeks. For this Week 24 interim analysis, the proportion of subjects with plasma HIV-1-RNA <50 was derived using the FDA Snapshot algorithm in the intent to treat exposed (ITT-E) population. Safety was assessed in all subjects who received study drug. An independent committee adjudicated IRIS episodes. The study was not powered to show a difference between study arms; no formal statistical hypothesis was tested.
Of 113 subjects enrolled, 69 were randomised to DTG and 44 to EFV. Median baseline HIV-1 RNA and CD4+ cell counts were 5.10 log10 c/mL and 208 cells/µL in the DTG arm and 5.24 log10 c/mL and 202 cells/µL in the EFV arm; 40% were women. The proportions of subjects with HIV-1-RNA <50 c/mL at Week 24 were 56/69 (81%) (95% CI: 72%, 90%) in the DTG arm and 39/44 (89%) (95% CI: 79%, 98%) in the EFV arm. The lower DTG response rate was driven by non-treatment related snapshot failures: five participants (7%) in DTG arm and none in EFV arm discontinued due to non-treatment-related reasons (loss to follow-up/protocol deviations). Median CD4+ cell increases at Week 24 were 146 cells/µL (IQR: 71, 214) for DTG and 93 cells/µL (IQR: 47, 178) for EFV. Two subjects discontinued study treatment due to AEs (both on EFV). TB-Associated IRIS rates (adjudicated and investigator reported) were low (DTG, n=4 [6%]; EFV, n=4 [9%]). No subjects discontinued due to IRIS or liver events.
Interim Week 24 results from this ongoing study show that DTG 50 mg twice daily appears to be effective and well-tolerated in HIV/TB co-infected adults receiving RIF-based TB therapy. Rates of IRIS were low. There were no new toxicity signals for DTG and no discontinuations due to liver events. These data support the use of DTG based regimen in HIV/TB co-infection.
Authors
Dooley KE, Kaplan R, Mwelase T, Grinsztejn B, Ticona E, Lacerda M, Cahn P, Belonosova E, Ait-Khaled M, Angelis K, Brown D, Singh R, Talarico C, Tenorio A, Aboud M
Abstract 2
Once-weekly isoniazid (INH) and rifapentine (RPT) (wHP) for 3 months is a recommended regimen for latent tuberculosis infection (LTBI). Limited drug interaction data exist on the use of this regimen with antiretroviral agents. This study sought to characterize the effects of wHP on the steady-state pharmacokinetics (PK) of dolutegravir (DTG).
This was an open-label, intrasubject drug interaction study in HIV-negative healthy volunteers comprised of 2 phases: (1) DTG once daily alone and (2) DTG once daily with wHP. The study design is detailed in Figure 1. DTG levels were measured at all PK visits, and RPT and INH levels on Day 19. DTG, RPT, and INH PK parameters were determined by non-compartmental methods (Phoenix WinNonlin, v6.4). Geometric mean ratios with 90% confidence intervals [CI] were compared between PK days. Adverse events (AEs) were graded via the DAIDS AE Toxicity Table (v2.0).
Of 4 enrolled subjects (3 males, 1 female, age 22-46 years), 3 completed the study and 1 withdrew prior to the 3rd dose of HP. The study was stopped prematurely due to the development of multiple AEs in 2 subjects. In both subjects, flu-like syndrome with symptoms of nausea, vomiting, and fever (Grades 2 and 3) began ~8 hours after the last doses of DTG, RPT, and INH and lasted 24-48 hours. One subject required a 24-hour hospitalization for management of orthostatic hypotension (Grade 3). Transaminase elevations (Grades 2-4) occurred in both subjects. Following wHP initiation, DTG exposure was decreased by 46% on Day 14 vs. 4 (p=0.134, 90% CI [0.27-1.10]) and Cmin was decreased by 74% on Day 15 (p=0.017) (n=4). The Cmin was 5.3x DTG's protein-adjusted IC90 (0.064 μg/mL) at this time point (range 0.9-11.0). One subject had multiple Cmin values <0.3 μg/mL following wHP initiation, a level associated with higher rates of DTG treatment failure. Day 19 exposure to RPT and its active metabolite were similar to reference PK data, but INH exposure was 67-92% higher than expected in the 2 subjects who developed AEs.
Serious toxicities, possibly related to high INH exposure, were observed in 2 of 3 subjects receiving 3 doses of wHP with once daily DTG, leading to early termination of our study. Limited PK data from these subjects showed decreased DTG exposure and Cmin values with wHP co-administration. Given that flu-like syndrome was reported in <4% of subjects in studies of the efficacy of wHP alone, these data suggest that co-administration of DTG and wHP should be avoided.
Authors
Kristina M Brooks, Alice K Pau, Jomy M George, Raul Alfaro, Anela Kellogg, Mary McLaughlin, Maryellen McManus, Colleen Hadigan, Joseph A Kovacs, Parag Kumar
JAID abstract
Background: Cotreatment of tuberculosis (TB) and HIV among coinfected patients is now the standard of care. Rifampin (RIF) is a standard part of TB treatment but is a potent inducer of drug metabolizing enzymes. This study evaluated the effect of RIF or rifabutin (RBT) on the pharmacokinetics of the investigational HIV integrase inhibitor, dolutegravir (DTG).
Methods: Phase I pharmacokinetic drug interaction study. In arm 1, healthy subjects received 50 mg of DTG once daily for 7 days (period 1), then 50 mg of DTG twice daily for 7 days (period 2), then 50 mg of DTG twice daily together with 600 mg of RIF once daily for 14 days (period 3). In arm 2, subjects received 50 mg of DTG once daily for 7 days (period 1) then 50 mg of DTG once daily together with 300 mg of RBT once daily for 14 days (period 2). PK sampling was performed at the end of each period.
Results: In arm 1, comparing period 3 to period 1, the geometric mean ratio (GMR) for the 24-hour area under the time–concentration curve (AUC0–24) was 1.33 [90% confidence interval (CI): 1.14 to 1.53], and the GMR for the trough (Cτ) was 1.22 (90% CI: 1.01 to 1.48). Comparing period 2 to period 1 in arm 2, the GMR for the AUC0–24was 0.95 (90% CI: 0.82 to 1.10), and the GMR for the Cτ was 0.70 (90% CI: 0.57 to 0.87).
Conclusions: Regimens including twice-daily DTG and RIF or once-daily DTG and RBT may represent a new treatment option for patients who require concomitant treatment of HIV and TB.
Authors
Dooley, Kelly E; Sayre, Patrick; Borland, Julie; Purdy, Elizabeth; Chen, Shuguang; Song, Ivy; Peppercorn, Amanda; Everts, Stephanie; Piscitelli, Stephen; Flexner, Charles
Clinical Infectious Diseases abstract
Background: Weekly rifapentine plus isoniazid for 3 months (3HP) is as effective as daily isoniazid for 9 months (9H) for latent tuberculosis infection in high-risk persons, but there have been reports of possible flu-like syndrome.
Methods: We identified clinically significant systemic drug reactions (SDR) and evaluated risk factors in patients who did not complete treatment in the PREVENT Tuberculosis study.
Results: Among 7552 persons who received ≥1 dose of study drug, 153 had a SDR: 138/3893 (3.5%) with 3HP vs 15/3659 (0.4%) with 9H (P < .001). In the 3HP arm, 87 (63%) had flu-like syndrome and 23 (17%) had cutaneous reactions; 13/3893 (0.3%) had severe reactions (6 were hypotensive) and 6 reported syncope. Symptoms occurred after a median of 3 doses, and 4 hours after the dose; median time to resolution was 24 hours. There were no deaths. In multivariate logistic regression analysis, factors independently associated with SDR included receipt of 3HP (adjusted odds ratio [aOR] 9.4; 95% confidence interval [CI], 5.5, 16.2), white non-Hispanic race/ethnicity (aOR 3.3; 95% CI, 2.3, 4.7), female sex (aOR 2.0; 95% CI, 1.4, 2.9), age ≥35 years (aOR 2.0; 95% CI, 1.4, 2.9), and lower body mass index (body mass index [BMI]; P = .009). In a separate multivariate analysis among persons who received 3HP, severe SDR were associated with white non-Hispanic race/ethnicity (aOR 5.4; 95% CI, 1.8, 16.3), and receipt of concomitant non-study medications (aOR 5.9; 95% CI, 1.3, 27.1).
Conclusions: SDR were more common with 3HP, and mostly flu-like. Persons of white race, female sex, older age, and lower BMI were at increased risk. Severe reactions were rare and associated with 3HP, concomitant medication, and white race. The underlying mechanism is unclear.
Authors
Timothy R Sterling, N Franklin Adkinson, Andrey Borisov, Jacques Grosset, Judith Hackman, Robert G Hamilton, M Elsa Villarino, Stephen Weis, Nong Shang, Fred Gordin, Awal Khan, Carol Dukes Hamilton, Dick Menzies, Amy Kerrigan, C Robert Horsburgh, Richard E Chaisson, George McSherry, Bert Arevalo, Andrew Vernon, David G Kleinbaum, Charles Heilig, Kimberly Fryer, Isabelle Sanchez, Suet K Lam, Nigel Scott, Ruth N Moro, Elizabeth Phillips, Gillian Shepherd, Christine Ho
[link url="http://www.croiconference.org/sessions/safety-and-efficacy-dolutegravir-based-art-tbhiv-coinfected-adults-week-24"]CROI 2018 abstract 1[/link]
[link url="http://www.croiconference.org/sessions/early-termination-pk-study-between-dolutegravir-and-weekly-isoniazidrifapentine"]CROI 2018 abstract 2[/link]
[link url="https://journals.lww.com/jaids/Abstract/2013/01010/Safety,_Tolerability,_and_Pharmacokinetics_of_the.4.aspx"]Journal of Acquired Immune Deficiency Syndrome abstract[/link]
[link url="https://www.viivhealthcare.com/media/press-releases/2018/march/viiv-healthcare-announces-positive-new-dolutegravir-data-for-the-treatment-of-people-living-with-hiv-co-infected-with-tuberculosis.aspx"]ViiV Healthcare material[/link]
[link url="https://www.healio.com/infectious-disease/hiv-aids/news/in-the-journals/%7Bcf814c2a-334b-45cb-98c3-3c9f1645c316%7D/combining-hiv-drug-dolutegravir-with-tb-therapy-causes-serious-toxicities"]Healio report[/link]
[link url="https://academic.oup.com/cid/article/61/4/527/329374"]Clinical Infectious Diseases abstract[/link]
