 A woman with advanced breast cancer which had spread around her body has been completely cleared of the disease by a ground-breaking therapy that harnessed the power of her immune system to fight the tumours. Researchers are now planning full-scale clinical trials.
A woman with advanced breast cancer which had spread around her body has been completely cleared of the disease by a ground-breaking therapy that harnessed the power of her immune system to fight the tumours. Researchers are now planning full-scale clinical trials.
The Guardian reports that it is the first time that a patient with late-stage breast cancer has been successfully treated by a form of immunotherapy that uses the patient’s own immune cells to find and destroy cancer cells that have formed in the body.
Judy Perkins, an engineer from Florida, was 49 when she was selected for the radical new therapy after several rounds of routine chemotherapy failed to stop a tumour in her right breast from growing and spreading to her liver and other areas. At the time, she was given three years to live.
Doctors who cared for the woman at the US National Cancer Institute in Maryland said Perkins’s response had been “remarkable”: the therapy wiped out cancer cells so effectively that she has now been free of the disease for two years.
“My condition deteriorated a lot towards the end, and I had a tumour pressing on a nerve, which meant I spent my time trying not to move at all to avoid pain shooting down my arm. I had given up fighting,” Perkins said. “After the treatment dissolved most of my tumours, I was able to go for a 40-mile hike.”
Laszlo Radvanyi, scientific director of the Ontario Institute for Cancer Research, who was not involved in Perkins’s treatment, is quoted in the report as saying it was “an unprecedented response in such advanced breast cancer.”
The dramatic success has raised hopes that the therapy will work in more patients with advanced breast cancer and other difficult to treat cancers, such as ovarian and prostate. Researchers are now planning full scale clinical trials to assess how effective the treatment could be.
“We are now at the cusp of a major revolution in finally realising the elusive goal of being able to target the plethora of mutations in cancer through immunotherapy,” Radvanyi said.
But, the report says, experts caution that the treatment has only proved itself in one woman and that the clinical trials are needed to see how effective the therapy could be in other cancer patients. Researchers point out that while the treatment could in principle work for many different kinds of cancer, it will not help everyone.
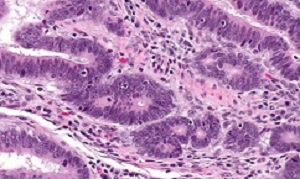
To create the treatment, doctors first cut small pieces of tissue from Perkins’s tumours and studied the DNA to find mutations specific to her cancer. They focused on mutations that disrupted four genes which produced an array of abnormal proteins in the tumours.
Next, the doctors extracted immune cells known as tumour infiltrating lymphocytes, or TILs, from the tumour biopsies. These are cells from the patient’s immune system that have invaded the tumour in a bid to kill it, but which failed in the task by being either too weak or too few in number.
After growing billions of these immune cells in the lab, the researchers screened them to find which ones would most effectively find and destroy the woman’s cancer cells by recognising their abnormal proteins.
The doctors treated Perkins by injecting 80bn of the carefully-selected immune cells into her body. The therapy was given alongside pembrolizumab, a standard drug that can help the immune system to attack cancers. Tests after 42 weeks showed Perkins was completely cancer free. She has remained so ever since.
The report says while the US doctors who developed the therapy cannot be sure how much the infused immune cells contributed to her recovery, the use of pembrolizumab alone has not been very effective for advanced breast cancer in the past. The infused T cells were found in Perkins’s system for at least 17 months after her treatment began.
The success is all the more remarkable because breast cancers, like prostate and ovarian cancer, have relatively few mutations, which makes them harder for the immune system to spot amid the body’s healthy tissues.
Alan Melcher, professor of translational immunotherapy at the Institute of Cancer Research in London, who was not involved in the study said in the report: “The work shows that even cancers like breast cancer, which don’t have many antigens, are amenable to this sort of treatment. It would certainly be applicable in principle to a range of tumours, and even those in which immunotherapy hasn’t worked so well yet.”
But Melcher points out that the therapy is complex and expensive and more importantly, requires doctors to find enough infiltrating immune cells in a patient’s tumour to make the treatment effective. “The case with other TIL therapies in the past is that they’ve not been able to expand enough T cells in many patients, there aren’t enough to start with.”
Simon Vincent, director of research at Breast Cancer Now, added: “This is a remarkable and extremely promising result, but we need to see this effect repeated in other patients before giving hope of a new immunotherapy for incurable metastatic breast cancer.
“Metastatic breast cancer remains incurable, and if we are to finally stop women dying we urgently need to find new ways to target and stop the spread of the disease. We are thrilled by this early finding, but we must remember that this type of immunotherapy remains an experimental approach that has a long way to go before it might be routinely available to patients.”
Abstract
Immunotherapy using either checkpoint blockade or the adoptive transfer of antitumor lymphocytes has shown effectiveness in treating cancers with high levels of somatic mutations—such as melanoma, smoking-induced lung cancers and bladder cancer—with little effect in other common epithelial cancers that have lower mutation rates, such as those arising in the gastrointestinal tract, breast and ovary1,2,3,4,5,6,7. Adoptive transfer of autologous lymphocytes that specifically target proteins encoded by somatically mutated genes has mediated substantial objective clinical regressions in patients with metastatic bile duct, colon and cervical cancers8,9,10,11. We present a patient with chemorefractory hormone receptor (HR)-positive metastatic breast cancer who was treated with tumor-infiltrating lymphocytes (TILs) reactive against mutant versions of four proteins—SLC3A2, KIAA0368, CADPS2 and CTSB. Adoptive transfer of these mutant-protein-specific TILs in conjunction with interleukin (IL)-2 and checkpoint blockade mediated the complete durable regression of metastatic breast cancer, which is now ongoing for >22 months, and it represents a new immunotherapy approach for the treatment of these patients.
Authors
Nikolaos Zacharakis, Harshini Chinnasamy, Mary Black, Hui Xu, Yong-Chen Lu, Zhili Zheng, Anna Pasetto, Michelle Langhan, Thomas Shelton, Todd Prickett, Jared Gartner, Li Jia, Katarzyna Trebska-McGowan, Robert P Somerville, Paul F Robbins, Steven A Rosenberg, Stephanie L Goff, Steven A Feldman
[link url="https://www.theguardian.com/science/2018/jun/04/doctors-hail-world-first-as-womans-advanced-breast-cancer-is-eradicated"]The Guardian report[/link]
[link url="https://www.nature.com/articles/s41591-018-0040-8"]Nature Medicine abstract[/link]
