 HIV/Aids remains the most common cause of death in the 47 nations of sub-Saharan Africa (SSA) but with striking geographic variations in prevalence, shows a precision mapping study by the Institute for Health Metrics and Evaluation. Some 5.3m South Africans under the age of 50 are HIV-positive, with Western Cape prevalence the lowest at 10% and KwaZulu-Natal the highest at 24%, reaching 30% in Pietermaritzburg.
HIV/Aids remains the most common cause of death in the 47 nations of sub-Saharan Africa (SSA) but with striking geographic variations in prevalence, shows a precision mapping study by the Institute for Health Metrics and Evaluation. Some 5.3m South Africans under the age of 50 are HIV-positive, with Western Cape prevalence the lowest at 10% and KwaZulu-Natal the highest at 24%, reaching 30% in Pietermaritzburg.
The paper reveals striking variation in HIV prevalence at provincial and district levels. The paper provides precise geographic estimates of HIV prevalence and numbers of people living with HIV to identify priority areas for health care support to reduce the burden of HIV.
“Changing the trajectory of HIV/Aids in Africa requires that we continue to seek better ways to know the epidemic. This paper will support policymakers and health care providers in locating hot-spots of HIV/Aids at national and sub-national levels, and will help guide smart investment of scarce resources for diagnosis, prevention, and treatment,” said Dr John Nkengasong, director of the Africa Centres for Disease Control and Prevention (Africa CDC).
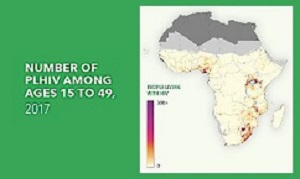
The study, conducted at the Institute for Health Metrics and Evaluation (IHME) at the University of Washington, is the first to map HIV prevalence among adults ages 15-49 comprehensively at a granular, subnational level for all 47 countries in sub-Saharan Africa. The results show high variation in prevalence and changes in prevalence over time within countries.
Since 2015, the World Health Organisation has recommended ART for all people living with HIV, because early treatment enables them to live longer and healthier lives and reduces the potential for transmitting the virus. Despite the rapid scale-up of ART, 34% of people in East and Southern Africa and 60% of people in West and Central Africa living with HIV are not currently on treatment, according to UNAIDS. Growing population size and continued high incidence of HIV infection, combined with increased life expectancy among people living with HIV (PLHIV), has led to an increase in PLHIV in sub-Saharan Africa: between 2000 and 2017, the number of people aged 15-49 years living with HIV in sub-Saharan Africa increased by 3m, even as HIV prevalence declined.
“Global funding for HIV/Aids has declined since 2013, but our research shows the substantial burden that still exists and reveals where geographically targeted interventions might make a big difference. Our goal is to provide robust data that can be used to help prevent future infections and ensure appropriate care for people living with HIV,” said IHME’s Dr Laura Dwyer-Lindgren, lead author and assistant professor of Health Metrics Sciences.
Key findings from the study include: most countries (36 of 47) had a more than two-fold difference in prevalence between second-level administrative subdivisions (such as districts or departments) in 2017 (Figure 1). In one-fourth of countries, the largest difference was more than five-fold; while the country-level analysis shows a clear divide between countries in southern sub-Saharan Africa and the rest of the continent, sub-national-level analysis reveals areas outside southern sub-Saharan Africa with high HIV prevalence, including parts of Kenya, Malawi, Uganda, and Tanzania where prevalence exceeded 10% in 2017 (Figure 1c); both the direction and rate of change in HIV prevalence from 2000 to 2017 varied between and within countries, highlighting the changing landscape and underscoring the need for current, local data; and the spatial concentration of people living with HIV (PLHIV) was highly variable. While a large number of PLHIV were concentrated in a small number of areas, an equally large number were widely distributed in areas with lower spatial concentrations of PLHIV.
The Bill & Melinda Gates Foundation funded the study, part of a five-year grant that enables IHME researchers and collaborators globally to map a range of health metrics in 5×5 square kilometre units.
The research is part of the Local Burden of Disease project at IHME led by Dr Simon I Hay, director of geospatial science at IHME and professor of health metrics sciences at the University of Washington.
The estimates highlight transnational trends, suggesting that international collaboration could help address persistent high prevalence in some areas. “The work done at IHME and on the Local Burden of Disease team is supported by a large network of collaborators, who play a critical role in the analysis of data and the use of published data in policy. We are always seeking to build our collaborative network and are very grateful to all who contributed to this study,” said Hay.
The paper builds on many previously published analyses, incorporating a broad array of data sources and presenting the results in a publicly accessible web-based visualization tool.
Almost one in five (17%) of South African adults aged between 15 and 49 have HIV – a five percentage point increase from 2000, reports The Times. A total of 5.3m South Africans under the age of 50 are HIV-positive, according to the study.
IHME tried to break down the number of people living with HIV across 46 African countries to help policymakers focus their efforts on fighting the epidemic.
The report says the study found South Africa’s HIV adult prevalence rate was much higher than most other countries, including Kenya (5.6%), Nigeria (3%), Namibia (13.8%), Zimbabwe (13.5%) and Mozambique (11.9%). But South Africa’s high rate is partly because more people are living longer with HIV due to antiretroviral therapies.
University of the Witwatersrand professor Francois Venter said the epidemic was not worsening. “Seventeen percent sounds about right for South Africa. More people on HIV treatment are living longer.”
And, the report says, University of KwaZulu-Natal pharmacologist Andy Gray agreed. “I do not think South Africa’s epidemic is getting worse. Prevalence would also be expected to increase as mortality drops because of antiretroviral therapy. More persons living with HIV are living longer,” Gray said. “The more important figure is the incidence, or the number of new cases.”
Gray said localised data would “help us to focus on areas of greatest need and to identify ‘host-spots’ where specific groups might be missed”.
The report says other interesting data was: the highest prevalence in Africa was the uMgungundlovu District Municipality in KwaZulu-Natal where Pietermaritzburg is almost three in 10 (29.7%); the district municipality with the lowest percent of adults living with HIV is West Coast District Municipality which includes the towns of Malmesbury, Clanwilliam, Langebaan and St Helena Bay; in Johannesburg, almost half-a-million (466,000) adult residents between the ages of 15 and 49 have HIV; and KwaZulu-Natal has the most residents in that age bracket living with HIV – 1.4m.
The provinces with the highest prevalence rates in South Africa are Mpumalanga (20.9%), Free State (21.3%), and KwaZulu-Natal (24%). The Western Cape (10%), Northern Cape (11.5%) and Limpopo (13.2%) have the lowest rates.
[link url="http://www.healthdata.org/news-release/striking-differences-rates-hivaids-within-african-nations"]Health Data material[/link]
[link url="https://www.timeslive.co.za/news/south-africa/2019-05-27-half-a-million-adults-in-johannesburg-are-hiv-positive-new-study/"]The Times report[/link]
[link url="http://www.healthdata.org/infographic/local-burden-disease-hiv-prevalence"]Study[/link]
[link url="https://vizhub.healthdata.org/lbd/hiv"]Data visualisations[/link]
