The Western Cape can be assumed to have near 60% immunity, which approaches herd immunity levels. That should also be true for the rest of South Africa, writes Emeritus Professor Jonny Myers, an occupational health and public health medicine specialist in the Centre for Environmental and Occupational Health Research at the department of public health and family medicine at University of Cape Town.
There is a frequently expressed view that South Africa and, more generally, African countries have been substantially less affected by COVID-19 than northern hemisphere developed countries. For South Africa, this is despite expectations to the contrary, because of our higher prevalence of HIV, TB, diabetes and other chronic morbidities. Is this really true? Did we in South Africa get off lightly with the COVID-19 epidemic from a health perspective in terms of severity of COVID-19 disease and mortality?
Myers writes: Analysis of the best available data indicates that in fact South Africa had a fairly severe epidemic, on a par with many developed countries. Analysis of the best data from northern countries, a season ahead of us in the course of the pandemic, provides some idea of what we can expect next. South Africa’s particular circumstances and patterns of immunity also provide some clues as to what may lie ahead. The good news is that we appear to have attained a fairly high degree of population immunity.
South Africa combines strong data capabilities, especially for an African country, with some sharply contrasting socioeconomic realities. There are substantial disparities in living conditions and administrative capabilities within and between provinces, cities, health districts and sub-districts. At provincial level, only the Western Cape combines highly functional public sector health services with excellent public health/epidemiological capabilities. In this province, health services were never overwhelmed, and accurate statistics about the epidemic were reported daily. On a national level, the South African Medical Research Council and the national civil registration system are world-class. Using data from these sources provides the best means of making comparisons between the epidemic in South Africa, and other countries and localities.
There is no reliable measure of the SARS-CoV-2 infection rate in any population globally. Case numbers confirmed as polymerase chain reaction (PCR) swab test positives depend upon the availability of testing capacity and the vagaries of testing policy, which varies substantially over time and by location. In the early part of the year there were severe test shortages globally. In the later part of the year in many locations there was much greater capacity, while testing criteria for members of the public have varied from time to time depending upon locality. Case numbers are consequently of little use for making comparisons.
PCR tests suffer from a considerable percentage (20%-30%) of false negatives arising from poor testing technique and the timing of testing. They are exquisitely sensitive and can produce false-positive results as they cannot distinguish between viable virus in the recently infected individual who may be asymptomatic but who is infectious to others and shedding virus, and non-viable viral fragments present in an asymptomatic individual who has recovered from an infection. This can lead to misidentification of a recovered case, no longer infectious, as an infectious case. Case numbers are consequently of little use for making comparisons.
Estimation of those who have been infected by SARS-CoV-2 based on serological testing for antibodies has been limited by early unavailability of reliable antibody tests (during epidemic peaks) and poor test performance. Most importantly, antibody concentrations wax and wane with time in individuals depending upon the time course of their infection, and hence also in the proportion of infected individuals in the population testing positive, depending upon the time course of the epidemic in that population. Antibody levels can take days or weeks after infection to become measurable, if at all, and can then decline rapidly and be undetectable some weeks after the infection. (This does not, however, mean that such individuals’ immunity has necessarily declined.) This time-dependence has been a major issue resulting in false positive and false negative tests that can be very misleading when making comparisons at different times and stages in the course of the infection in individuals, and the course of the epidemic in the population. Antibody prevalence in the population is typically low (1%-3%) before the epidemic peaks, at which time it is much higher (20%-50%), and then declines rapidly after the peak (below 5%). For this reason, epidemiological surveys conducted outside of the peak will often underestimate the true picture.
Despite all these uncertainties that frustrate ascertainment of the true infection rate, it is possible to compare the extent and time course of the different epidemics in different places by using a more robust indicator: reported confirmed COVID-19 deaths. However, even this metric has its problems, that have to do with what is written on the death certificate as the cause of death, and the efficiency of administrative recording and reporting.
A better option is to consider excess deaths, which are weekly deaths over and above what would be expected based on the average of deaths over the past several years for that week. Excess deaths, irrespective of their causes, are only available for a few, mainly developed, countries. They represent a gold standard of measurement for COVID-19 deaths, and constitute an upper limit on the real number of COVID-19 deaths during the epidemic period. Rates per 100,000 of population make the figures comparable across different countries.
The proportion of excess deaths that can be attributed to reported COVID-19 deaths can also be compared across and within countries. In the case of South Africa, this proportion is only credible for the Western Cape Province, at 70% (the figure of confirmed COVID-19 cases accounts for 70% of excess deaths). For the other provinces and nationally, proportions range between 17-36%, which are extremely low by global standards, and indicate substantial under-counting of COVID-19 deaths for the other eight provinces and the country as a whole.
So, how has South Africa done compared with other countries?
It should be noted that comparisons made here make use of crude mortality rates which are not standardised for age, which is the biggest predictor of COVID-19 mortality by far. As South Africa has a younger population distribution than any of the comparator populations in the tables that follow below, its age-adjusted excess death rate would be even higher by comparison with the others than what is shown.
A comparison of the most reliable indicator of the severity of the epidemic of all – excess deaths per 100,000 population – reveals that South Africa as a whole is in the same company as several northern hemisphere developed countries, and it is immediately apparent that South Africa has by no means got off lightly with a mild epidemic, despite claims that this is so by, among others, international news reporters, local experts advising the government, and some mathematical modelling pundits.
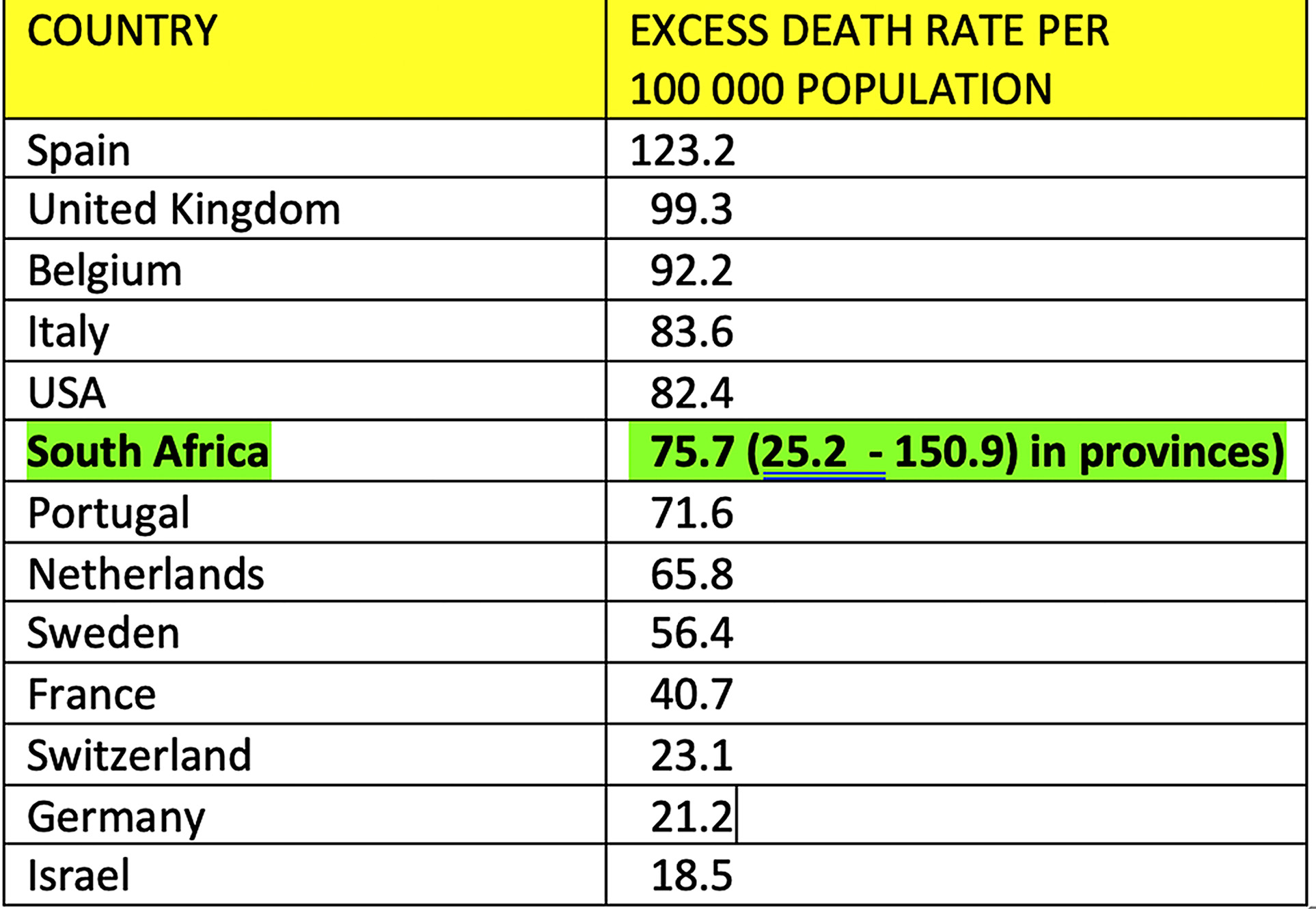
Drilling down to the provincial level in South Africa, the most affected province is the Eastern Cape, with a rate of 150.9 excess deaths per 100,000, and the least affected province is Limpopo, with 25.2 per 100,000, a six-fold difference. However, despite this sharp contrast, both are comparable with the developed countries in the table above. There can be no claim of South African beneficial experience exceptionalism here. The bad news is that we have had as severe an epidemic as have some of the worst affected countries globally.
As stated, reported COVID-19 deaths in the Western Cape constitute about 70% of excess provincial deaths, which is a lower bound for the true COVID-19 mortality. The real percentage must be higher, and the overwhelming majority (between 80% and 90% or higher) of excess deaths during the period of the South African epidemic must have been caused by COVID-19, even if a minority of excess deaths could be attributed to, for example, fear of infection causing people with other potentially fatal conditions to avoid health services, to die prematurely.
Less reliably, we can compare reported official COVID-19 deaths per 100,000 population. We are 27th globally, according to Worldometer.
.
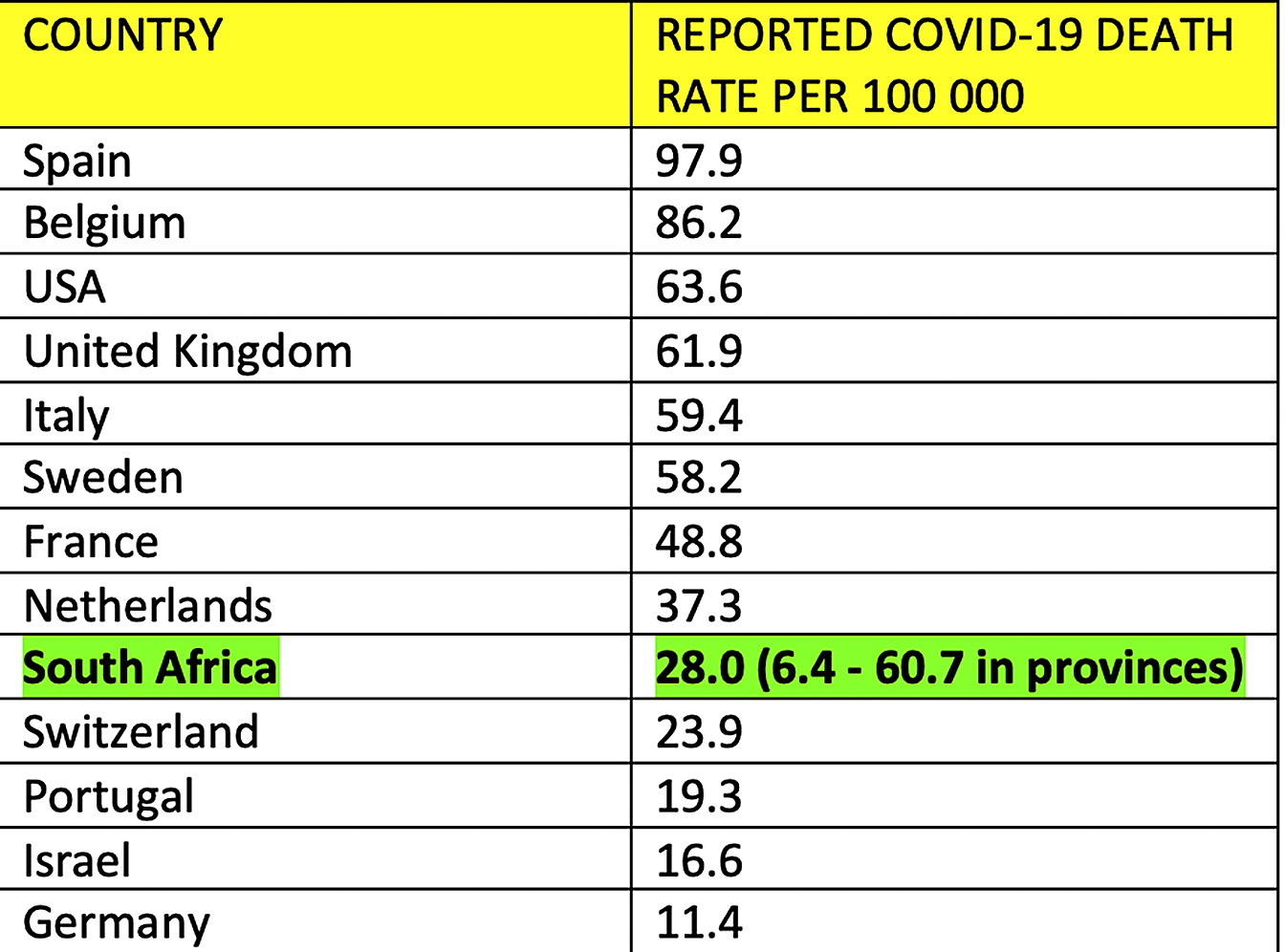
Drilling down again to provincial level in South Africa, the most affected province by this less than perfect metric of official reported COVID-19 death rates is the Western Cape, with a rate of 60.7 per 100,000, and the least affected province is Limpopo, with 6.4 per 100,000, a tenfold difference. The Western Cape provincial rate is similar to the worst affected developed countries in the table above. Reported deaths have been shown throughout the epidemic to have been severely undercounted, due to administrative problems in all South African provinces other than the Western Cape. Despite this, South Africa has still not been shown to have a surprisingly low death rate, even using South African reported COVID-19 deaths.
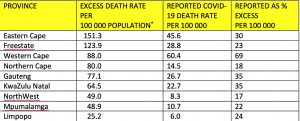
For the Western Cape, which has the most accurate COVID-19 death statistics in South Africa, the excess provincial death rate is 88.1 per 100,000, and the reported provincial COVID-19 death rate is 60.7 per 100,000. Both of these rates are averages across the province. Comparative COVID-19 death rates in the health districts and subdistricts of the Western Cape are not in the public domain. As the province contains disparities in wealth and health, including formal and informal housing areas, death rates for the poor and disadvantaged areas are likely to be higher than more affluent areas, as has been the case in other countries experiencing the pandemic. This puts the death rates in poor and disadvantaged areas of the country in the company of the worst affected countries globally.
These rates show that there is no mysteriously low COVID-19 death rate in South Africa. On the contrary, South Africans have death rates comparable to the worst affected northern developed European countries. By extension, the same should apply to other low- and middle-income countries in Africa, and elsewhere with similar patterns of densely populated urban areas and informal housing settlements.
What can we expect about the future course of the pandemic in South Africa?
South Africa has experienced a mature epidemic, as evidenced by the decline in both cases and deaths. As in other countries, there is now some concern about an impending second wave of the pandemic. This has reference to the 1918-1920 flu epidemic in which a more severe second wave of deaths in August to December 1918 targeting young adults followed the first milder wave from March to July 1918, which targeted the very young and very old. The relevance of this reference to the COVID-19 pandemic is questionable for many reasons, principal among them that neither influenza viruses nor antibiotics had yet been discovered in 1918-1920, and that likely bacterial pneumonia superinfection was untreatable.
Six months in, it is possible to make some observations about the course of the COVID-19 pandemic in different parts of the world, and the effectiveness of various national and regional responses. The data indicate that non-pharmaceutical interventions (NPIs), specifically lockdowns, may delay the surge, depending upon their severity level and timing.
Lockdown as the most extreme form of NPI was promoted almost accidentally, in that the pandemic originated in China and came naturally to an authoritarian government with full societal control. Other countries followed suit. Thus, action against COVID-19 has been mostly suppressionist in character from the beginning.
Apart from this most severe form of interruption of viral transmission, the other NPIs are mitigatory in nature, and may reduce transmission to varying degrees, allowing for fewer infections and lower infectious doses (smaller inocula of virus), leading to fewer infections and milder disease.
The beneficial effects of suppression of transmission come at the expense of retaining large numbers of susceptibles in the population. Total suppression, as in China or New Zealand, results in a small initial surge with an abrupt decline to zero cases and subsequent deaths. This leaves the remaining population almost entirely susceptible to any future infection outbreak. A totally uncontrolled spread of the virus reduces the number of susceptibles rapidly, leading to a peak and then decline of the daily death curve over a relatively short period of time. A more controlled spread of the virus using NPIs would lead to a slower growth with a lower surge peak, perhaps plateauing over a longer period of time, leading to higher levels of population immunity with smaller and fewer subsequent surges and ultimately, herd immunity. This is the trade-off.
In the case of very large jurisdictions (the US, India, Brazil, Russia, the EU), the epidemic takes considerable time to spread to the entire population. This can span seasons, and the virus propagates differently according to population density, travel networks, popularity of destination, and variably effective measures to reduce the impact of the virus. While parts of the US and Europe have experienced an early rapid epidemic, other parts of these countries and more remote destinations within them are experiencing later epidemic surges in both cases and deaths. Worries about future surges as the northern winter approaches are most pronounced now in northern developed countries which experienced early mature epidemics. There are many reports and indeed signs of increased viral activity after a long quiescent period now that the autumn is here.
The role of immunity to the virus is key to understanding what comes next. Immunity at both individual and population levels has proved very difficult to measure. Immunity there must be, otherwise there would be no recoveries, and the epidemic would not wane in countries that have not implemented NPIs (declines have been seen in Brazil and other countries notorious for not using NPIs).
But there are no simple tests of immune status available that could be applied at either individual or population level. Meaningful tests would need to be able to measure innate immunity (especially in children), cross-immunity to past coronavirus infections (SARS1, MERS, common cold coronaviruses), trained non-specific immunity due to prior vaccination against other diseases (MMR, BCG), and specific immunity to SARS-CoV-2 (not only B-cell humoral antibody responses, but also T-cell based cellular responses). Measurements of only one aspect of specific immunity (typically, antibody prevalences in populations), especially at early or late stages of the pandemic, have often been widely misinterpreted as indicating very low population immunity compared with a level that could confer herd immunity, causing the virus to disappear (estimated to be around 60% immune individuals in a population). If there is 40% seropositivity for antibodies to SARS-cov-2 in a random sample of adult, and you add 100% immunity in children who make up about 28% of the population (these I consider to be all immune as they do not get seriously ill or die), you get 60%.
The EU can broadly be divided into Western and Eastern Europe and their epidemic patterns have been different. Western countries have experienced early severe epidemics relatively unresponsive to NPIs with late lockdowns, while Eastern countries have experienced initially milder epidemics which have in many cases been more responsive to NPIs with early lockdowns. As the northern winter approaches there are different visible patterns of the re-emergence of viral activity. Also, with time, much has been learned about medical treatment in hospitals and mortality rates have declined.
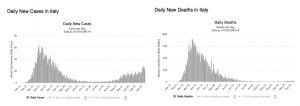
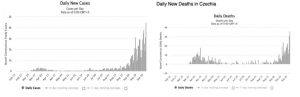
Italy and other Western European countries like the UK, France and Spain, show a second surge in cases but not deaths, while Czechia and other Eastern European countries show maturing epidemics with delayed first surges in both cases and deaths after initial suppression by early lockdown and NPIs.
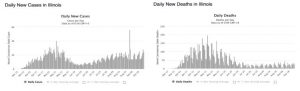
The US is a vast country encompassing 51 “countries” (including Washington DC) at different stages of their epidemics. As of 26 September, half the states have had early epidemics, while 25 are having late epidemics as the pandemic crosses the country. Fifteen, or just over half, of the 26 early epidemic states are currently experiencing what have been referred to as “casedemics”. These are surges in daily cases without corresponding surges in daily deaths, even accounting for the lag between cases and deaths. An example is Illinois, which experienced an early relatively uncontrolled mature epidemic. Lately there has been a resurgence in cases, but not deaths.
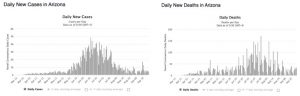
In places like Arizona, which are experiencing a delayed or later epidemic, the first surge in cases matches the subsequent surge in deaths.
The UK, Italy, Spain and France and many states in the US are examples of “casedemics” with second surges in cases but as yet no corresponding surge in deaths. So, the good news is that there is little evidence as at the time of writing of any second substantial surge of COVID-19 deaths in the US or Europe amounting to a feared second wave after the initial maturation of the epidemic in a first wave, despite the panic in the media. What is most likely to be happening is that localities that have had a mature epidemic have a higher population immunity, perhaps approaching herd immunity, with the most vulnerable in their populations having already died. Due to the current easy availability of testing, unlike the early stages where testing capability was more limited, many asymptomatics and mildly affected cases are now being found among the younger, healthier sections of populations, with lower risk of severe disease. These individuals are busily building population immunity to herd immunity levels in these sections of the population through increased socialisation after lockdown, reintegration in the workplace and attendance at educational institutions. Others at higher risk are likely to have changed their behaviours and shielded more carefully, while improved medical interventions have resulted in lower death rates even for those at increased risk. This should prevent death surges anywhere near as substantial as the first wave in localities that have experienced either early or delayed mature epidemics.
How does this apply to South Africa? As we have seen above, South Africa has experienced a mature epidemic as severe as most in the northern hemisphere earlier this year, and is unlikely to have a greater proportion of susceptibles than, say New York State, which has as yet experienced no second surge in either cases or deaths.
What is the likely state of our population immunity? Antibody test positive prevalences near 40% at the peak of the local epidemic were found among women at public sector antenatal clinics and attendees at HIV clinics in the Western Cape. This represents a more or less random sample of the population. Add to this the 20% or more of children in the population who are immune to COVID-19 via other mechanisms, and the Western Cape can be assumed to have near 60% immunity, which approaches herd immunity levels. The presence of additional unmeasured cellular immunity in adults with negative antibody tests has not even been taken into account in this simple calculation. Further evidence lies in the virtually trouble-free school re-openings in the Western Cape. Schools have experienced no shutdowns, and there has been no spike in provincial case numbers. This may paradoxically have something to do with testing policy that limits its use as a routine daily precondition for entering the workplace or schools. Might this be a benefit of NOT “testing, testing, testing” – the panicky mantra heard so frequently in the global media?
What is true for the Western Cape should also apply to the rest of South Africa, as the epidemics in the other provinces have followed the Western Cape in quick succession and have all peaked and declined in similar manner.
The prospects for a severe resurgence, or what is often termed a second wave, in South Africa, which has experienced a severe mature epidemic (a first wave), do not seem very likely.
Lastly a word of caution. This analysis is based on average data currently available at the date of writing. There is still some considerable heterogeneity in the number of likely susceptibles in different localities. There are likely to be more susceptibles in the formal housing sector areas. Caution is still advised for shielding the elderly and those with relevant comorbidities. Young people are doing good work by building population immunity by transmitting virus at low levels to other young and healthy people. They are doing the job of vaccination at a time when we do not have vaccines and will most likely not have these for another year or so. Vaccination may also be of doubtful efficacy and timeliness.
Meanwhile, the young and healthy must just take care not to transmit infections to the elderly and those with comorbidities which put them at risk.
This analysis was also published in Daily Maverick