Since a 1913 New York Times headline read: “Marvellous cures of cancer attributed to radium”, the field of radiation oncology has developed countless innovations to harness radiotherapy to reduce suffering, preserve organs, and help save the lives of countless patients with cancer.
In 2023, unedited headlines in leading newspapers have read: “Rectal cancer patients could be spared the brutal effects of radiation” and “More women with breast cancer could skip harsh radiation, study says”.
By using adjectives such as brutal and harsh, these headlines sadly propagate and amplify fears and misconceptions regarding radiotherapy that research has shown to be unfounded and that negatively affect patient care, write oncology experts Dr Narek Shaverdian and Dr Reshma Jagsi in JAMA Network.
The treatment of cancer benefits from an ever-growing selection of therapies that now includes chemotherapy, targeted drugs, immunotherapy, radio-pharmaceuticals, minimally invasive surgery, and ablative tumour treatments.
However, unique to radiotherapy are inherent fears and unknowns that are easily reinforced and triggered.
Radiation is associated with the brutality of war, evacuations, natural disasters, and birth defects. These recent headlines lean into these fears and suggest that unlike other cancer therapies, radiotherapy mostly harms and must be avoided.
What is often missed – and should be clear – is the profound benefit of modern radiotherapy.
When appropriately used, it can allow patients with sarcomas to undergo limb-sparing surgery, patients with breast cancer to preserve their breasts with breast conservation therapy, patients with lung cancer unfit to undergo surgery the ability to be cured with non-invasive stereotactic body radiotherapy (SBRT), patients with head and neck cancers the ability to save their voices, and patients with invasive and fungating tumours, much-needed symptom relief.
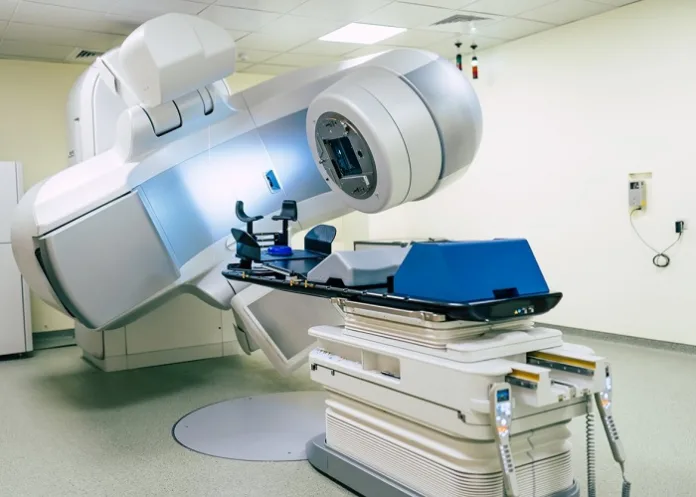
Indeed, since 1913, the field of radiation oncology has tirelessly developed advanced methods to precisely target tumours while sparing normal tissues, improve efficacy, reduce adverse effects, and improve the treatment experience.
Specifically, patients with breast, lung, and prostate cancer once required up to eight weeks of daily radiation for adjuvant or definitive treatment but now can receive treatment in five to seven days or less, based on numerous trials that have evaluated approaches of accelerated partial breast radiotherapy, ultra-hypofractionated radiotherapy, and SBRT.
Where prior treatments were limited by the ability to target moving structures, image-guided radiation treatments now offer continuous visualisation and adaptive targeting of the tumour, as seen in recent trials evaluating use of magnetic resonance imaging–guided radiotherapy for prostate, liver, and pancreatic cancers.
Newer methods of radiotherapy, such as intensity modulation, protons, and SBRT, allow shaping of radiation fields and ranges to avoid critical structures and to deliver higher doses of radiation where needed and very little where not.
Specific examples include proton therapy to reduce the dose – to normal tissues – that causes toxic effects, and second, malignant neoplasms in paediatric patients, leading to dose distributions that contrast dramatically with previous approaches in settings such as cranio-spinal radiation, or SBRT for metastases to bones and spine that randomised trials have shown to offer patients durable pain and disease control.
Moreover, the unceasing effort to identify radiation-dose tolerances of normal organs has also allowed for reduced toxic effects with use of intensity-modulated radiotherapy or other advanced techniques.
These improvements include the ability to reduce xerostomia and improve quality of life by sparing the salivary glands and swallowing structures in patients with head and neck cancers, reduce cardiac and pulmonary late effects by limiting dose to the heart and lungs in patients with thoracic cancers, and improve cognitive outcomes by avoiding the hippocampus in patients with brain cancers.
Along with physicians, health journalists share the responsibility to communicate about cancer treatments clearly without bias, even if doing so leads to a less compelling headline.
Patients should not be scared off when they do have a clear net benefit from treatment. Regarding radiotherapy, the toxic effects are manageable and justified for the large benefit many patients receive.
Additionally, treatment decision-making is patient centred, allowing patients to reach personalised decisions with the aid of their treatment team.
For example, in patients with breast cancer, some may choose to omit radiotherapy without compromising their overall survival, if they are willing to accept the adverse effects of long-term anti-hormonal medications, and a higher risk of the cancer returning and requiring additional treatment.
Radiation oncologists are often themselves the leaders of such clinical trials, including one of the authors of this Viewpoint.
Sadly, the headline proclaiming, “More women with breast cancer could skip harsh radiation, study says”, misses the critical nuances and trade-offs involved. Such headlines do not accurately convey the results of quality-of-life studies that have shown that most patients with breast cancer tolerate radiotherapy with only mild adverse effects that resolve completely, noting that the experience was much better than anticipated.
Conversely, those who receive anti-hormonal medication can report serious and bothersome adverse effects for many years.
Similarly, the headline that claimed, “Rectal cancer patients could be spared the brutal effects of radiation”, failed to acknowledge that the more intensive and longer chemotherapy regimen the patients received in lieu of radiation resulted in a significant increase in acute toxic effects that must be considered when reaching personalised treatment decisions.
This headline disregarded the much more balanced interpretation by the study investigators that may not lead to as many clicks but also does not mislead in ways that may affect a patient’s future care decisions.
As oncologists, we have the privilege to care for patients during the most difficult and unimaginable time in their lives. We see the devastation, the pain, the suffering that cancer causes each day.
Like all physicians, we honour an ancient oath to do no harm.
We hope that our colleagues in all disciplines of oncology will join us in encouraging health reporters in the future to consider honouring a similar duty when they wield the tremendous power of the pen, which is demonstrably mightier than not only a sword but also a scalpel.
Dr Narek Shaverdian, Department of Radiation Oncology, Memorial Sloan Kettering Cancer Centre, New York.
Dr Reshma Jagsi, Department of Radiation Oncology, Emory University, Atlanta.
JAMA Oncology article – When Headlines Harm Patients With Cancer (Creative Commons Licence)
See more from MedicalBrief archives:
Rectal cancer patients could skip radiation: US trial
Faster breast cancer radiation treatment as effective as long course
Shorter radiation after mastectomy is safe and effective
Twice-daily radiation therapy cuts deaths from head and neck cancer