A recent Japanese medical team report describes a 63-year-old man who developed dysesthesia in his feet and was misdiagnosed with chronic inflammatory demyelinating polyradiculoneuropathy.
He was treated with intravenous immunoglobulin, but his sensorimotor polyneuropathy continued to worsen.
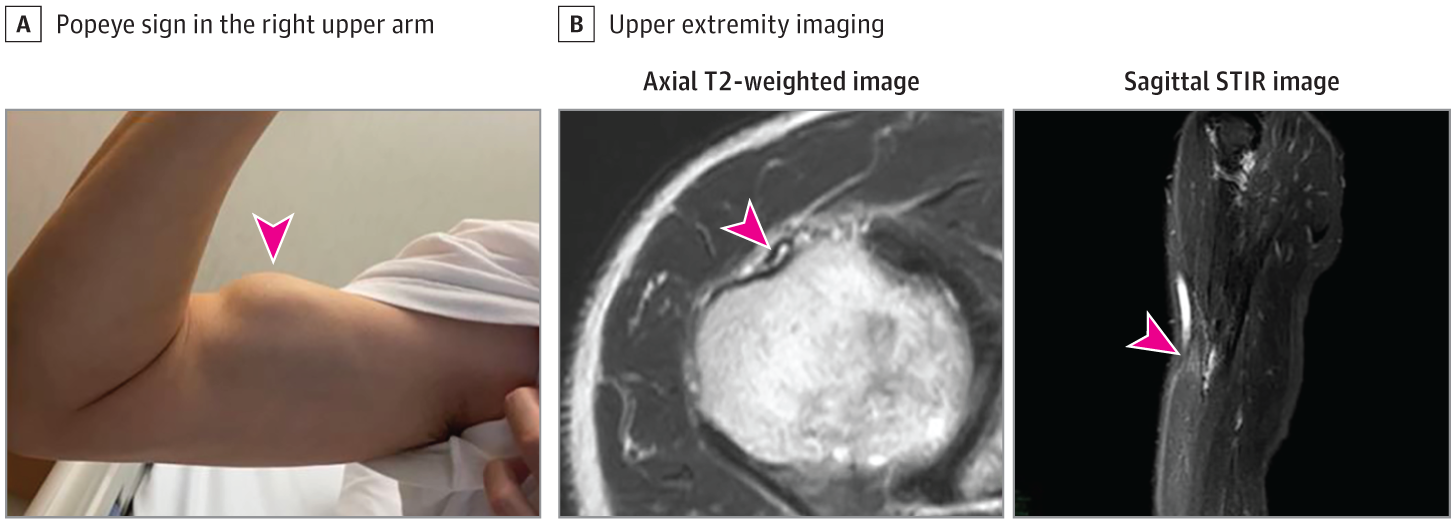
In their JAMA Neurology report, the team, lead by the Department of Neurology, Graduate School of Medical Sciences at Kumamoto University, wrote that physical examination revealed sensorimotor polyneuropathy and bulging bicep in his right upper arm – termed Popeye sign, often reportedly associated with the rupture of the long head of the bicep.
He had exhibited right bulging bicep since disease onset, and upper extremity magnetic resonance imaging revealed tendon degeneration and retraction of biceps brachii. A nerve conduction study confirmed axonal sensorimotor neuropathy affecting the lower limbs.
An endoscopic biopsy of the stomach demonstrated transthyretin (TTR)-positive amyloid deposits in vascular walls by Congo red and immunohistochemical staining. Genetic testing of TTR revealed a TTR Ala97Gly mutation.
He did not have a family history of the disease.
A transthoracic echocardiogram indicated left ventricular hypertrophy with a maximum wall thickness of 12.8 mm; technetium-labelled bone scintigraphy revealed myocardial slight uptake, thus suggesting cardiac amyloidosis.
He had no clinical findings associated with carpal tunnel syndrome, autonomic dysfunction, and ocular involvement.
He was diagnosed with late-onset hereditary amyloid transthyretin (ATTR) amyloidosis and was treated with patisiran, a TTR gene-silencing drug.
What is ATTR amyloidosis?
Hereditary ATTR amyloidosis is an inherited systemic amyloidosis that causes systemic symptoms, such as sensorimotor neuropathy, autonomic dysfunction, cardiomyopathy, gastrointestinal dysfunction, kidney failure and ocular disorders.
Researchers have reported on more than 150 mutations in the TTR gene, most of which are reportedly pathogenic.
The early diagnosis of hereditary ATTR amyloidosis is important because recently developed disease-modifying therapies, such as TTR tetramer stabilisers and TTR gene silencing therapies, reportedly halt disease progression.
However, patients with hereditary ATTR amyloidosis are diagnosed within six months in only 35% of the cases, besides being often misdiagnosed with chronic inflammatory demyelinating polyradiculoneuropathy, diabetic neuropathy, or lumbar spinal stenosis.
Particularly, most patients with late-onset hereditary ATTR amyloidosis do not have a family history of the disease and are commonly misdiagnosed with other diseases several years from the onset.
This novel report demonstrated Popeye sign in a patient with hereditary ATTR amyloidosis. Moreover, Popeye sign has been reported in approximately 30% of patients with wild-type ATTR amyloidosis, which is an ageing-related sporadic systemic amyloidosis caused by wild-type TTR.
It is supposedly important for diagnosing wild-type ATTR amyloidosis.
Generally, bicep tendon rupture is thought to be associated with tendon degeneration due to many etiologies, such as fluroquinolones, corticosteroids, mixed connective tissue disorders, and diabetes, in addition to overuse and kinetic load.
Histopathological findings of ruptured bicep tendon are not available in patients with ATTR amyloidosis. Although exact reasons why the bicep tendon was prone to rupture were undetermined in the present case, we speculated that his bicep tendon rupture was associated with tendon degeneration due to ATTR amyloid deposits, in addition to overuse and kinetic load.
Popeye sign may be uncommon in patients with hereditary ATTR amyloidosis; however, it can facilitate distinguishing hereditary ATTR amyloidosis from other peripheral neuropathies.
JAMA Neurology article – Popeye Sign in Hereditary Transthyretin Amyloidosis (Open access)
