Kendric Cromer, a 12-year-old boy in Washington, last week became the first person in the world with sickle cell disease to begin a commercially approved gene therapy that may cure the condition, and change his whole life.
For the estimated 20 000 people with sickle cell in the United States who qualify for the treatment, the start of Kendric’s months-long medical journey may offer hope. But it also signals the difficulties patients face as they seek new sickle cell treatments.
For a lucky few, like Kendric, the treatment could make possible lives they have longed for. A shy adolescent, he had learned that ordinary activities, like riding a bike, going outside on a cold day, playing soccer, could trigger episodes of searing pain.
Now, reports The New York Times, he feels as if he has a chance for a normal life.
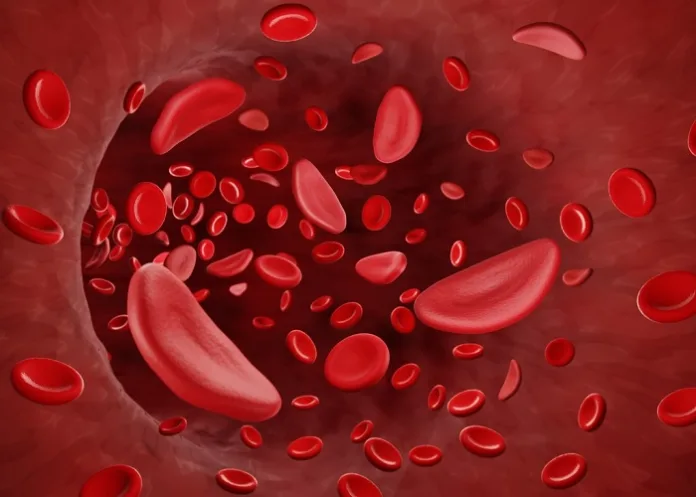
Near the end of last year, the US Food and Drug Administration gave two companies authorisation to sell gene therapy to people with sickle cell disease – the genetic disorder of red blood cells that causes debilitating pain and other medical problems.
About 100 000 people in the US have sickle cell, most of them black. People are born with the disease when they inherit the mutated gene for the condition from each parent.
The treatment helped patients in clinical trials, but Kendric is the first commercial patient for Bluebird Bio, a Massachusetts company. Another company, Vertex Pharmaceuticals of Boston, declined to say if it had started treatment for any patients with its approved CRISPR gene-editing-based remedy.
Kendric, whose family’s health insurance agreed to cover the procedure, began his treatment at Children’s National Hospital in Washington. Last week’s treatment was only the first step. Doctors removed his bone marrow stem cells, which Bluebird will then genetically modify in a specialised lab for his treatment.
That will take months. But before it begins, Bluebird needs hundreds of millions of stem cells from Kendric, and if the first collection – taking six to eight hours – is not sufficient, the company will try once or twice more.
If it still doesn’t have enough, Kendric will have to spend another month in preparation for another stem cell extraction.
Bluebird is charging $3.1m for its gene therapy – Lyfgenia. It’s one of the highest prices ever for a treatment.
The whole process is so involved and time-consuming that Bluebird estimates it can treat the cells of only 85 to 105 patients each year, and that includes not just sickle cell patients, but also patients with a much rarer disease – beta thalassemia – who can receive a similar gene therapy.
Medical centres also have the capacity to handle only a limited number of gene therapy patients. Each person needs expert and intensive care.
After a patient’s stem cells have been treated, the patient has to stay in the hospital for a month. For most of that time, they are severely ill from powerful chemotherapy.
Children’s National can accept only about 10 gene therapy patients a year.
“This is a big effort,” said Dr David Jacobsohn, chief of the hospital’s division of blood and marrow transplantation.
Top of the list
Bone marrow stem cells, the source of all the body’s red and white blood cells, are normally nestled in a person’s bone marrow. But Kendric’s doctors infused him with a drug, plerixafor, which pried them loose and let them float in his circulatory system.
To isolate the stem cells, medical staff inserted a catheter into a vein in his chest and attached it to an apheresis machine, a boxlike device next to his hospital bed. It spins blood, separating it into layers – a plasma layer, a red cell layer and a stem cell layer.
Once enough stem cells have been gathered, they will be sent to Bluebird’s lab, where technicians will add a healthy haemoglobin gene to correct the mutated ones that are causing his sickle cell disease.
They will send the modified cells back three months later. The goal is to give Kendric red blood cells that will not turn into fragile crescent shapes and get caught in his blood vessels and organs.
Despite the astronomical price and the gruelling process, there are waiting lists of patients hoping for relief from a disease that can cause strokes, organ damage, bone damage, agonising pain and shortened lives.
At Children’s National, Jacobsohn said at least 20 patients were eligible and interested. The choice of who would go first came down to who was sickest, and whose insurance came through.
Kendric qualified on both counts. But even though his insurance was quick to approve the treatment, the insurance payments are only part of what it will cost his family.
Chances and hopes
His mother, Deborah Cromer, a realtor, and her husband, Keith, who works in law enforcement, had no idea they might have a child with sickle cell.
They found out only when Deborah was pregnant with Kendric. Tests showed their baby would have a one-in-four chance of inheriting the mutated gene from each parent and having sickle cell disease.
They could terminate the pregnancy or take a chance. They decided to take a chance.
The news that Kendric had sickle cell was devastating.
He had his first crisis when he was three. Sickled blood cells had become trapped in his legs and feet. Their baby was inconsolable, in such pain that his mother couldn’t even touch him.
His parents took him to Children’s National.
The pain crises became more and more severe. It seemed as though anything could set them off – 10 minutes of playing volleyball, a dip in the pool. And when they occurred, Kendric sometimes needed five days to a week of treatment in the hospital to control his pain.
His parents always stayed with him. His mother slept on a narrow bench in the hospital room, his father slept in a chair.
Eventually the disease began wreaking severe damage. Kendric developed avascular necrosis in his hips – bone death that occurs when bone is deprived of blood. The condition spread to his back and shoulders. He began taking a large daily dose of gabapentin, a medicine for nerve pain.
His pain never let up. He became increasingly sedentary.
His parents began to hope for gene therapy, but when they found out what it would cost, they lost some of their hope.
However, their insurer approved the treatment in a few weeks, they said. Now it has begun, and Kendric is looking forward to the future.
He wants to be a geneticist.
See more from MedicalBrief archives:
UK first to approve CRISPR-based treatment for sickle cell disease
CRISPR treatment now approved for beta thalassemia
FDA approves sickle cell treatment but obstacles remain