Researchers have produced the first set of risk charts for 182 countries to predict their patients’ 10-year risk of cardiovascular disease (CVD).
These will be useful everywhere, but particularly in low- and middle-income countries that lack locally-developed models to predict CVD risk, and in places where access to labs that can perform bloodwork is limited. Typically, blood tests are necessary to measure CVD risk factors such as blood sugar and lipids.
Previously available risk models and charts were applicable only to a few high-income countries or to regions.
“National and international guidelines recommend that physicians use risk prediction equations, usually in the form of risk charts, to predict which of their patients are at high risk for heart disease and stroke, and to suggest lifestyle modification or prescribe medication to lower their risk. These new risk charts, specifically calibrated for each country, remove major obstacles in applying risk-based strategies to prevent cardiovascular diseases,” said Dr Goodarz Danaei, assistant professor of global health at Harvard Chan School and senior author of the paper.
Cardiovascular diseases are the leading cause of death and disability worldwide, and more than three-quarters of CVD-related deaths occur in low- and middle-income countries. But identifying those at high risk of having a future cardiovascular event can be difficult in many countries because there are no reliable risk charts, and because calculating risk typically relies on measurements of blood sugar and lipids – which, in resource-poor settings, can make the assessment too costly or impractical.
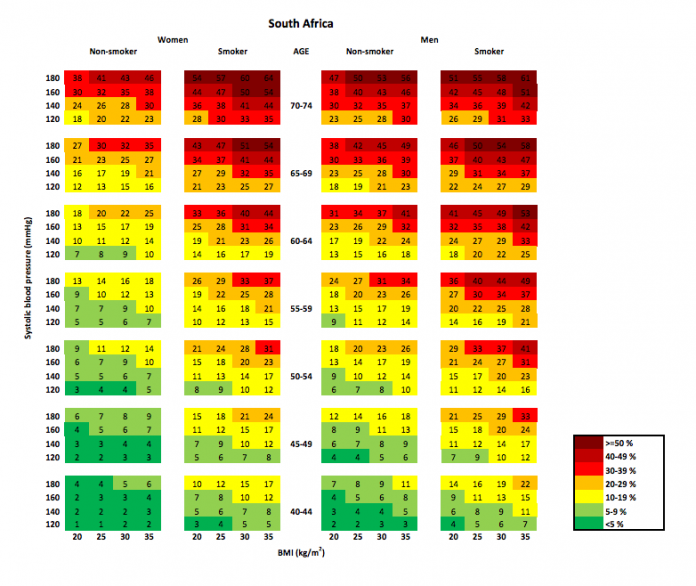
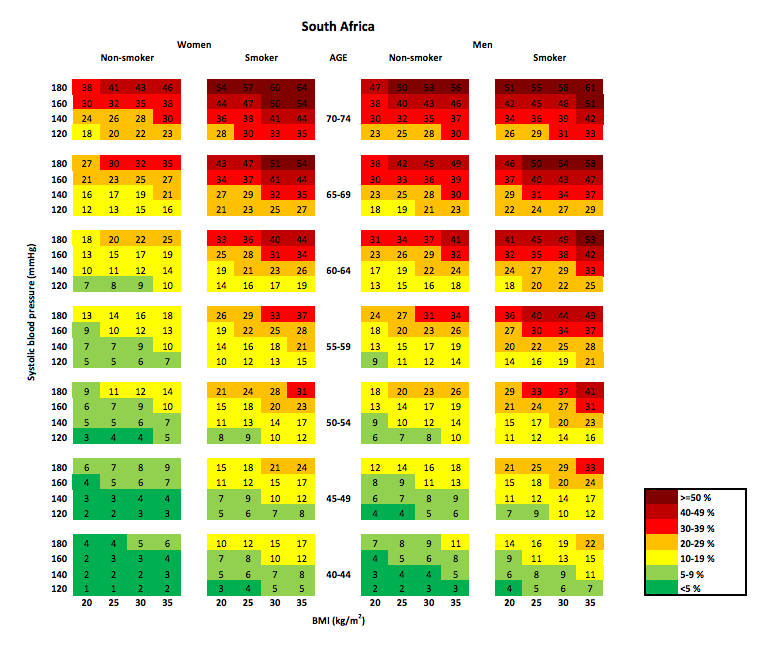
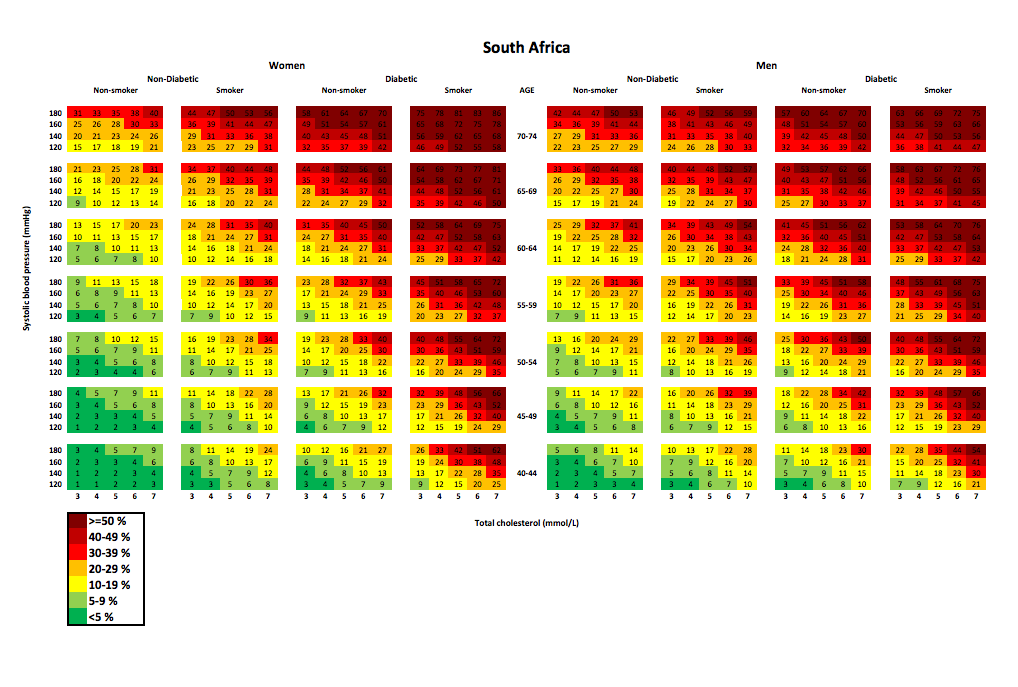
The researchers set out to provide CVD risk prediction models geared toward each country. They developed two models: one that uses lab-based blood measurements (a “laboratory-based model”), and one that can be used in the absence of bloodwork (an “office-based model”). To generate the models, researchers used data from eight long-term studies in the US and re-calibrated the models by using data on CVD risk factor levels and CVD rates for each target country.
The study found that, between 85% and 99% of the time, the office-based risk prediction model worked as well as the laboratory-based model in characterising CVD risk. However, among diabetes patients, the office-based model underestimated the risk noticeably.
The study also found that 10-year CVD risk was lower in high-income countries than in lower- and middle-income countries. The highest CVD risks were in countries in Central and Southeast Asia and in Eastern Europe. CVD risk also varied significantly across countries and across genders. For example, the proportion of people in high-income countries at high risk for CVD ranged from 1% for South Korean women to 42% for Czech men, and in low- and middle-income countries it ranged from 2% in Uganda for both men and women to 13% in Iranian men.
“Our results suggest that urgent action is needed to strengthen the primary health care system in many low- and middle-income countries to detect individuals at high risk of CVD and to provide lifestyle counseling or medications to lower their risk,” said Peter Ueda, postdoctoral research fellow in the department of global health and population at Harvard Chan and lead author of the study.
Summary
Background: Worldwide implementation of risk-based cardiovascular disease (CVD) prevention requires risk prediction tools that are contemporarily recalibrated for the target country and can be used where laboratory measurements are unavailable. We present two cardiovascular risk scores, with and without laboratory-based measurements, and the corresponding risk charts for 182 countries to predict 10-year risk of fatal and non-fatal CVD in adults aged 40–74 years.
Methods: Based on our previous laboratory-based prediction model (Globorisk), we used data from eight prospective studies to estimate coefficients of the risk equations using proportional hazard regressions. The laboratory-based risk score included age, sex, smoking, blood pressure, diabetes, and total cholesterol; in the non-laboratory (office-based) risk score, we replaced diabetes and total cholesterol with BMI. We recalibrated risk scores for each sex and age group in each country using country-specific mean risk factor levels and CVD rates. We used recalibrated risk scores and data from national surveys (using data from adults aged 40–64 years) to estimate the proportion of the population at different levels of CVD risk for ten countries from different world regions as examples of the information the risk scores provide; we applied a risk threshold for high risk of at least 10% for high-income countries (HICs) and at least 20% for low-income and middle-income countries (LMICs) on the basis of national and international guidelines for CVD prevention. We estimated the proportion of men and women who were similarly categorised as high risk or low risk by the two risk scores.
Findings: Predicted risks for the same risk factor profile were generally lower in HICs than in LMICs, with the highest risks in countries in central and southeast Asia and eastern Europe, including China and Russia. In HICs, the proportion of people aged 40–64 years at high risk of CVD ranged from 1% for South Korean women to 42% for Czech men (using a ≥10% risk threshold), and in low-income countries ranged from 2% in Uganda (men and women) to 13% in Iranian men (using a ≥20% risk threshold). More than 80% of adults were similarly classified as low or high risk by the laboratory-based and office-based risk scores. However, the office-based model substantially underestimated the risk among patients with diabetes.
Interpretation: Our risk charts provide risk assessment tools that are recalibrated for each country and make the estimation of CVD risk possible without using laboratory-based measurements.
Authors
Peter Ueda, Mark Woodward, Yuan Lu, Kaveh Hajifathalian, Rihab Al-Wotayan, Carlos A Aguilar-Salinas, Alireza Ahmadvand, Fereidoun Azizi, James Bentham, Renata Cifkova, Mariachiara Di Cesare, Louise Eriksen, Farshad Farzadfar, Trevor S Ferguson, Nayu Ikeda, Davood Khalili, Young-Ho Khang, Vera Lanska, Luz León-Muñoz, Dianna Magliano, Paula Margozzini, Kelias P Msyamboza, Gerald N Mutungi, Kyungwon Oh, Sophal Oum, Fernando Rodríguez-Artalejo, Rosalba Rojas-Martinez, Gonzalo Valdivia, Rainford Wilks, Jonathan E Shaw, Gretchen A Stevens, Janne Tolstrup, Bin Zhou, Joshua A Salomon, Majid Ezzati, Goodarz Danaei
[link url="https://www.hsph.harvard.edu/news/press-releases/cardiovascular-risk-tools/"]Harvard TC Chan School of Public Health material[/link]
[link url="http://www.thelancet.com/journals/landia/article/PIIS2213-8587(17)30015-3/fulltext"]The Lancet Diabetes & Endocrinology abstract[/link]
[link url="http://www.globorisk.org/news-and-media/new-tools-developed-help-clinicians-predict-risk-cardiovascular-disease"]Risk Charts[/link]