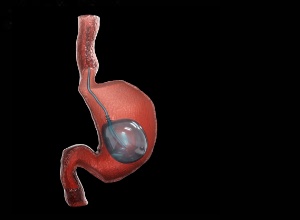
With obesity affecting 40% of the US population, the American Gastroenterological Association (AGA) has released new recommendations on the therapeutic role of intragastric balloons (IGBs), reports MedPage Today. These devices have been associated with significant improvements in weight loss over and above non-invasive standard of care (SOC) approaches.
"There is a vast area of unmet need with respect to weight-loss interventions, as only 1.1% of eligible patients with obesity are receiving primary bariatric surgery," wrote an expert panel led by Dr Thiruvengadam Muniraj, of Yale University School of Medicine in New Haven, Connecticut.
For those for whom traditional weight loss strategies fail, IGBs have been seen to yield greater weight loss, improve metabolic laboratory abnormalities, and positively change the trajectory of several obesity-related comorbidities, the panel noted in the new clinical practice guideline.
MedPage Today reports that with respect to weight loss, IGBs led to greater weight loss at 6, 9, and 12 months after initial placement compared with patients treated with SOC alone, the document states. The amount of weight loss incrementally decreased, however, for each successive time period.
"Clearly IGB therapy (with lifestyle modification) is superior to lifestyle modifications alone at initial and maintenance of weight loss for patients in the short term (within at least 12 months of initial IGB placement)," the panelists wrote.
While endoscopic bariatric therapies have evolved as an attractive tool for weight loss, fewer than 5% of obesity patients seeking weight loss therapy are aware of endoscopic options, Muniraj said in an AGA statement. "Our hope is that this new guideline can lead to shared decision-making between patients and providers to determine if intragastric balloons are the best weight loss option for that individual patient."
After reviewing the evidence and considering the balance between harms and benefits, as well as costs and patient preferences, the AGA panelists made the following key recommendations:
Obesity patients seeking a weight loss intervention should consider using IGB therapy to augment the effect of moderate- to high-intensity lifestyle modifications: to minimise the risk of gastrointestinal bleeding, patients undergoing IGB therapy should be treated with prophylactic proton pump inhibitors; during IGB placement, patients should receive intraoperative anaesthetics associated with a low incidence of nausea and afterward continue anti-emetic medication for 2 weeks; while perioperative screening for nutritional deficiencies is not required, IGB recipients should take one or two multivitamins after placement; and to keep weight off after IGB removal, dietary interventions, pharmacotherapy, repeat IGB, or bariatric surgery are advised, with the maintenance strategy determined using a shared decision-making approach.
"None of these recommendations is likely to be controversial among gastroenterologists, but it is important to stress that IGBs are an adjunct to the cornerstone of weight loss, which is lifestyle modification," Muniraj is quoted in MedPage Today as saying.
As for specific IGB type, the panel said fluid-filled balloons may promote greater weight loss but at the cost of lower tolerability and a less favourable safety profile compared with their gas-filled counterparts. Again, collaborative decision-making should be the approach in choosing a balloon device.
"Shared decision-making is a critical component of obesity therapy – for everything from selecting the right IGB device to what concomitant lifestyle modifications, pharmacotherapy, or sequential procedures a patient should pursue," Muniraj said.
In reviewing the literature, the panel found five randomised controlled trials and 18 observational studies showing that IGBs lowered both haemoglobin A1c and fasting blood glucose levels significantly more than use of non-invasive therapy alone.
In particular, improved laboratory profiles were observed in obesity patients who had a fasting blood glucose level greater than 100 mg/dL, hemoglobin A1c over 6.5%, and a body mass index over 40.
Mixed results emerged for lipid profiles, however. Although there was no reduction in triglycerides, there was a trend to decreasing low-density lipoproteins with IGBs, the panel members found.
Liver function test abnormalities also improved, with alanine aminotransferase values decreasing by 9 U/L and aspartate aminotransferase values dropping by 3 U/L.
Finally, diabetes, hypertension, and dyslipidaemia all retreated to a statistically significant greater degree with IGB as opposed to non-invasive weight loss. And patients who used IGBs reduced their waist circumference by 4.1 cm compared with those who used non-invasive approaches.
"Taken together, current data suggest that IGB therapy improves laboratory abnormalities and accomplishes greater rates of remission for several medical diseases associated with obesity than SOC alone," MedPage Today reports the AGA authors concluded.
Study details
AGA Clinical Practice Guidelines on Intragastric Balloons in the Management of Obesity
Thiruvengadam Muniraj, Lukejohn W Day, Levi M Teigen, Edith Y Ho, Shahnaz Sultan, Perica Davitkov, Raj Shah, M Hassan Murad
Published in Gastroenterology on 1 April 2021
Abstract
Obesity is a global pandemic, affecting about 40% of adults in the United States. There is a vast area of unmet need with respect to weight-loss interventions, as only 1.1% of eligible patients with obesity are receiving primary bariatric surgery. Endoscopic bariatric therapies have evolved as an attractive tool for weight loss; however, <5% of patients with obesity seeking a weight-loss therapy are aware of endoscopic weight-loss options. Intragastric balloons (IGBs) launched nearly 4 decades ago have recently gained more popularity with multiple new devices introduced into the US market. Although IGBs are a plausible option for patients seeking weight loss, it is essential for providers, patients, and health care teams to understand how IGBs can augment the effect of lifestyle modifications with respect to important patient outcome measures, such as weight loss, improving metabolic parameters, and minimizing comorbid medical conditions. At the same time, it is also important for providers and patients to be aware of the adverse events and tolerability associated with IGBs, given that the devices have evolved over the years and newer models are available in the US market. This guideline can assist both patients and providers in determining whether IGB is a weight-loss option that should be considered and/or pursued in patients with obesity.