 Building on research results showing patients with larger ischaemic strokes could benefit from endovascular thrombectomy, an international, multi-centre Phase III clinical trial will be starting at The University of Texas Health Science Centre at Houston (UTHealth). The trial, called SELECT2 (Optimising Patient Selection for Endovascular Treatment in Acute Ischemic Stroke), is a randomised, controlled, open-label, assessor-blinded trial assessing efficacy and safety of thrombectomy procedure in patients with larger ischaemic stroke.
Building on research results showing patients with larger ischaemic strokes could benefit from endovascular thrombectomy, an international, multi-centre Phase III clinical trial will be starting at The University of Texas Health Science Centre at Houston (UTHealth). The trial, called SELECT2 (Optimising Patient Selection for Endovascular Treatment in Acute Ischemic Stroke), is a randomised, controlled, open-label, assessor-blinded trial assessing efficacy and safety of thrombectomy procedure in patients with larger ischaemic stroke.
While multiple previous clinical trials showed that endovascular thrombectomy was safe and beneficial for patients with smaller areas of damage from an ischaemic stroke, potential safety and benefits for larger strokes are still unknown.
Ischaemia refers to blood supply restriction to tissue. In an ischaemic stroke, a clot blocks blood flow in a cerebral artery, preventing oxygen from reaching the surrounding brain tissue and resulting in cell death. That area of cell death is called an ischaemic core.
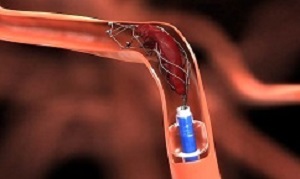
In endovascular thrombectomy, a small catheter is guided through an artery, usually a femoral artery, through the body to the site of the blockage in the brain. A blood clot removal device is deployed, which captures the clot. The catheter is then retracted.
The earlier Phase II clinical trial (SELECT), which enrolled patients in nine US comprehensive stroke centres, included 105 patients with large ischaemic cores. It showed potential benefits: 31% of patients who were treated with endovascular thrombectomy achieved functional independence, compared to 14% of patients who received medical management only.
"It is unclear now if thrombectomy is safe and efficacious in patients with a large ischaemic core stroke. Treating physicians face a dilemma on whether to intervene in these patients," said Dr Amrou Sarraj, first and corresponding author and associate professor of neurology at McGovern Medical School at UTHealth. "Our results represent very good preliminary data that thrombectomy may be safe and efficacious in this population. It's time to test those results in a randomised trial."
The results of SELECT showed reasonable safety outcomes with thrombectomy in patients with larger strokes. The risk of secondary bleeding with thrombectomy did not increase significantly compared to medical management. Mortality rate decreased with thrombectomy (29%) as compared to medical management (42%).
The Phase III trial, which begins in August, will enrol 560 patients at 30 comprehensive stroke centres in the US, Canada, and Europe.
"If proven to be safe and effective, SELECT2 will extend thrombectomy indications to improve clinical outcomes in a large group of patients that does not have many treatment options at this point," said Sarraj, who is a member of UTHealth Institute for Stroke and Cerebrovascular Disease.
Abstract
Importance: The efficacy and safety of endovascular thrombectomy (EVT) in patients with large ischemic cores remains unknown, to our knowledge.
Objective: To compare outcomes in patients with large ischemic cores treated with EVT and medical management vs medical management alone.
Design, Setting, and Participants: This prespecified analysis of the Optimizing Patient’s Selection for Endovascular Treatment in Acute Ischemic Stroke (SELECT) trial, a prospective cohort study of imaging selection that was conducted in 9 US comprehensive stroke centers, enrolled patients between January 2016 and February 2018, and followed them up for 90 days. Patients with moderate to severe stroke and anterior circulation large-vessel occlusion presenting up to 24 hours from the time they were last known to be well were eligible for the cohort. Of these, patients with large ischemic cores on computed tomography (CT) (Alberta Stroke Program Early CT Score <6) or CT perfusion scanning (a volume with a relative cerebral blood flow <30% of ≥50 cm3) were included in analyses.
Exposures: Endovascular thrombectomy with medical management (MM) or MM only.
Main Outcomes and Measures: Functional outcomes at 90 days per modified Rankin scale; safety outcomes (mortality, symptomatic intracerebral hemorrhage, and neurological worsening).
Results: A total of 105 patients with large ischemic cores on either CT or CT perfusion images were included: 71 with Alberta Stroke Program Early CT Scores of 5 or less (EVT, 37; MM, 34), 74 with cores of 50 cm3 or greater on CT perfusion images (EVT, 39; MM, 35), and 40 who had large cores on both CT and CT perfusion images (EVT, 14; MM, 26). The median (interquartile range) age was 66 (60-75) years; 45 patients (43%) were female. Nineteen of 62 patients (31%) who were treated with EVT achieved functional independence (modified Rankin Scale scores, 0-2) vs 6 of 43 patients (14%) treated with MM only (odds ratio [OR], 3.27 [95% CI, 1.11-9.62]; P = .03). Also, EVT was associated with better functional outcomes (common OR, 2.12 [95% CI, 1.05-4.31]; P = .04), less infarct growth (44 vs 98 mL; P = .006), and smaller final infarct volume (97 vs 190 mL; P = .001) than MM. In the odds of functional independence, there was a 42% reduction per 10-cm3 increase in core volume (adjusted OR, 0.58 [95% CI, 0.39-0.87]; P = .007) and a 40% reduction per hour of treatment delay (adjusted OR, 0.60 [95% CI, 0.36-0.99]; P = .045). Of 10 patients who had EVT with core volumes greater than 100 cm3, none had a favorable outcome.
Conclusions and Relevance: Although the odds of good outcomes for patients with large cores who receive EVT markedly decline with increasing core size and time to treatment, these data suggest potential benefits. Randomized clinical trials are needed.
Authors
Amrou Sarraj, Ameer E Hassan, Sean Savitz, Clark Sitton, James Grotta, Peng Chen, Chunyan Cai, Gary Cutter, Bita Imam, Sujan Reddy, Kaushik Parsha, Deep Pujara, Roy Riascos, Nirav Vora, Michael Abraham, Haris Kamal, Diogo C. Haussen, Andrew D Barreto, Maarten Lansberg, Rishi Gupta, Gregory W Albers
[link url="https://www.uth.edu/news/story.htm?id=a2c84594-d729-444a-ae87-cb01cb94d2ca"]University of Texas Health Science Centre at Houston material[/link]
[link url="https://jamanetwork.com/journals/jamaneurology/article-abstract/2738511"]JAMA Neurology abstract[/link]
