 Insulin pumps do not take away the need for vital education on diabetes self-management and were no more effective than injections in helping adults with type 1 diabetes control their blood sugar levels, reports UK National Institute for Health Research (NIHR)-funded research.
Insulin pumps do not take away the need for vital education on diabetes self-management and were no more effective than injections in helping adults with type 1 diabetes control their blood sugar levels, reports UK National Institute for Health Research (NIHR)-funded research.
The REPOSE trial, funded by the NIHR and led by Professor Simon Heller of the University of Sheffield and Sheffield Teaching Hospital's NHS Foundation Trust, found that barriers to successful diabetes control cannot be overcome by providing additional technology in the form of insulin pumps.
Type 1 diabetes is a lifelong condition affecting around 250,000 people in the UK. It occurs when the immune system destroys the cells that make insulin – the hormone needed to control blood sugar levels. Many people with type 1 diabetes struggle to achieve blood sugar level targets and a significant proportion go on to develop serious complications, reducing the length and quality of their lives.
To minimise potentially life-threatening complications caused by high blood sugars, patients take multiple daily shots of insulin and as the body is no longer to produce the insulin itself, the dose must be adjusted to fit with regular food intake and exercise.
Alongside this, patients attend the Dose Adjustment For Normal Eating (DAFNE) educational programme. This has been shown to improve diabetes control, reduce risks of low blood sugars and improve quality of life.
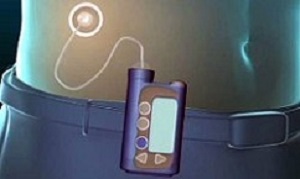
However, newer forms of technology, including insulin pumps which continuously supply insulin using a device that sits under the skin, are becoming more widely available, with six per cent of adults with type 1 diabetes estimated to insulin pumps, a figure that rises to 40% in the US.
The use of pumps is expensive, but can provide patients with a more flexible way of delivering their insulin. Until now, little research has been done to see how effective the pump is compared with injections.
During the research Heller and his team allocated 267 participants (at eight centres across England and Scotland) onto a week-long educational course to learn about flexible insulin therapy, and split them into two groups. One group also received training on how to use a pump to deliver their insulin while the second group used multiple insulin injections for two years.
Although, participants using the pumps were more satisfied with the treatment, the findings reveal that there were no significant benefits in quality of life between those using insulin pumps and those taking daily shots of insulin.
Hellersaid: “Offering pumps to adults whose blood glucose levels are high and who have not yet received training in insulin self-management doesn’t appear to offer additional benefit.
“What the results do suggest is that ensuring people receive training to enable them to better manage their diabetes is likely to be more beneficial. Pumps may be useful in patients who are highly engaged in their own management, but find that the limitations of insulin treatment prevent them achieving their glucose targets.”
Andy Broomhead, 35, of Chapeltown, Sheffield, took part in the Repose trial. He believes education is the key when learning how to control type 1 diabetes: “Taking part in a DAFNE course as part of the REPOSE trial changed my life. DAFNE gave me the freedom, flexibility and confidence to manage my own Type 1 diabetes confidently for the first time in a decade. I now feel empowered to look after myself and it's made me feel more confident living with Type 1 diabetes every day.
“Whilst it can be hard to put up with checking my own blood glucose seven or eight times a day, calculating carbohydrate values and then deciding how much insulin I need to give myself for every meal, I know how important it is to get those things right. DAFNE has given me the skills I need to look after my own health and I'd encourage anyone who hasn't yet been on the course to do so.”
Dr Martin Ashton-Key, scientific director at the NIHR Evaluation Trials and Studies Coordinating Centre, added “The findings of this NIHR-funded research will be of real value to patients with diabetes and clinicians in the NHS.”
Abstract
Objective: To compare the effectiveness of insulin pumps with multiple daily injections for adults with type 1 diabetes, with both groups receiving equivalent training in flexible insulin treatment.
Design: Pragmatic, multicentre, open label, parallel group, cluster randomised controlled trial (Relative Effectiveness of Pumps Over MDI and Structured Education (REPOSE) trial).
Setting: Eight secondary care centres in England and Scotland.
Participants: Adults with type 1 diabetes who were willing to undertake intensive insulin treatment, with no preference for pumps or multiple daily injections. Participants were allocated a place on established group training courses that taught flexible intensive insulin treatment (“dose adjustment for normal eating,” DAFNE). The course groups (the clusters) were then randomly allocated in pairs to either pump or multiple daily injections.
Interventions: Participants attended training in flexible insulin treatment (using insulin analogues) structured around the use of pump or injections, followed for two years.
Main outcome measures: The primary outcomes were a change in glycated haemoglobin (HbA1c) values (%) at two years in participants with baseline HbA1c value of ≥7.5% (58 mmol/mol), and the proportion of participants achieving an HbA1c value of <7.5%. Secondary outcomes included body weight, insulin dose, and episodes of moderate and severe hypoglycaemia. Ancillary outcomes included quality of life and treatment satisfaction.
Results: 317 participants (46 courses) were randomised (156 pump and 161 injections). 267 attended courses and 260 were included in the intention to treat analysis, of which 235 (119 pump and 116 injection) had baseline HbA1c values of ≥7.5%. Glycaemic control and rates of severe hypoglycaemia improved in both groups. The mean change in HbA1c at two years was −0.85% with pump treatment and −0.42% with multiple daily injections. Adjusting for course, centre, age, sex, and accounting for missing values, the difference was −0.24% (−2.7 mmol/mol) in favour of pump users (95% confidence interval −0.53 to 0.05, P=0.10). Most psychosocial measures showed no difference, but pump users showed greater improvement in treatment satisfaction and some quality of life domains (dietary freedom and daily hassle) at 12 and 24 months.
Conclusions: Both groups showed clinically relevant and long lasting decreases in HbA1c, rates of severe hypoglycaemia, and improved psychological measures, although few participants achieved glucose levels currently recommended by national and international guidelines. Adding pump treatment to structured training in flexible intensive insulin treatment did not substantially enhance educational benefits on glycaemic control, hypoglycaemia, or psychosocial outcomes in adults with type 1 diabetes. These results do not support a policy of providing insulin pumps to adults with poor glycaemic control until the effects of training on participants’ level of engagement in intensive self management have been determined.
Authors
REPOSE study group
[link url="https://www.sheffield.ac.uk/news/nr/insulin-pumps-no-real-benefit-1.693035"]University of Sheffield material[/link]
[link url="http://www.bmj.com/content/356/bmj.j1285"]BMJ abstract[/link]
