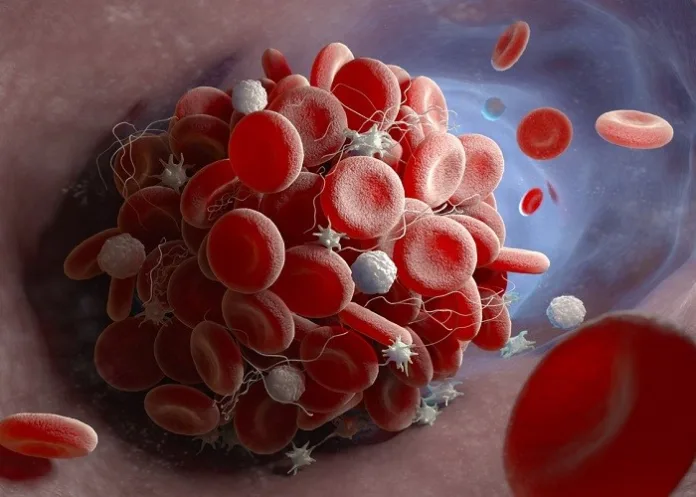
Researchers have suggested there is a small, increased risk of blood clots when taking common painkillers while on the Pill, and that women should be informed of the link between non-steroidal anti-inflammatory drugs (NSAIDs) and hormonal contraception.
The Danish study, led by the University of Copenhagen and published in The British Medical Journal (BMJ), included data for more than 2m women, and found that the risk was greater in women using ibuprofen, diclofenac and naproxen while on combined pills containing progesterone and oestrogen.
But it was smaller in women using progestogen-only pills – often dubbed the mini-pill – implants and coils, reports the Daily Mail.
The researchers used national medical records to track diagnoses of venous thromboembolism among 2m women aged 15 to 49 living in Denmark between 1996 and 2017, with no history of blood clots, cancer, hysterectomy or fertility treatment.
Hormonal contraception was divided into high, medium and low risk, according to their links with clots in previous studies.
The researchers said high risk, hormonal contraception included combined pills containing either 50mcg oestrogen or third or fourth generation progestogen, while medium risk included all other combined oral contraceptives.
Low or no risk included the mini pill, implants and coils.
The study found that NSAIDs were used by 529 704 women on hormonal contraception, with ibuprofen being the most frequently used NSAID (60%), followed by diclofenac (20%) and naproxen (6%).
Over an average of 10 years, 8 710 venous clots occurred (2 715 pulmonary embolisms and 5 995 deep venous thromboses), and 228 (2.6%) women died within 30 days of diagnosis.
NSAID use was associated with four extra venous thromboembolic events per week per 100 000 women not using hormonal contraception, 11 extra events in women using medium risk hormonal contraception, and 23 extra in women using high risk hormonal contraception.
The link was strongest for diclofenac compared with ibuprofen and naproxen, the paper found.
However, the experts warned that the study did not prove a link but said women should be given information about the risks.
A range of factors that could influence the results, such as age, education level, pregnancy history, prior surgery, high blood pressure and diabetes, were taken into account when analysing the findings.
Dr Channa Jayasena, clinical senior lecturer and consultant in reproductive endocrinology and andrology, Imperial College London, said: “Blood clots are dangerous because they can lodge in the lungs, causing breathing and heart problems.
“Contraceptive medications and painkillers like ibuprofen are essential for many women to avoid pregnancy and cope with period pain, and both of them can occasionally cause serious side effects.
“But I don't think this study alone should put off women taking either the pill, painkillers, or both if needed.”
Dr Ian Musgrave, senior lecturer in the faculty of medicine at the University of Adelaide, said: “The way the study was reported can give rise to unwarranted concern.
“The conclusion that ‘NSAID use was positively associated with the development of venous thromboembolism in women of reproductive age’ was only true for the high risk group: the medium group risk was the same as the women on no hormonal contraception, and for the low risk group the risk may even be less.
“The risk of clotting events in women in the high-risk hormonal group who used NSAIDs was around 1.5 times that of women who used NSAIDs but did not use hormonal contraceptives.
“The strength of the study is the large nation-wide coverage, linked to extensive medical databases so NSAID use could be effectively monitored, and avoids the bias of people trying to recall how much of a medication they used.
“Only 0.4% of the population had a clotting event, and the small numbers affect the robustness of the result.”
Nonetheless, he added, the study provides good evidence that women on hormonal contraception “who are at high risk of clotting events have an increased risk when on NSAIDs, and prescribing pain relief for them should recognise this”.
He said what was not clear from this study was “how long you need to be taking NSAIDs before the risk was increased”.
Study details
Venous thromboembolism with use of hormonal contraception and non-steroidal anti-inflammatory drugs: nationwide cohort study
Amani Meaidi, Annamaria Mascolo, Christian Torp-Pedersen, et al.
Published in The BMJ on 6 September 2023
Abstract
Objective
To study the influence of concomitant use of hormonal contraception and non-steroidal anti-inflammatory drugs (NSAIDs) on the risk of venous thromboembolism.
Design
Nationwide cohort study.
Setting
Denmark through national registries.
Participants
All 15-49-year-old-women living in Denmark between 1996 and 2017 with no medical history of any venous or arterial thrombotic event, cancer, thrombophilia, hysterectomy, bilateral oophorectomy, sterilisation, or infertility treatment (n=2 029 065).
Main outcome measures
A first time discharge diagnosis of lower limb deep venous thrombosis or pulmonary embolism.
Results
Among 2.0m women followed for 21.0m person years, 8710 venous thromboembolic events occurred. Compared with non-use of NSAIDs, use of NSAIDs was associated with an adjusted incidence rate ratio of venous thromboembolism of 7.2 (95% confidence interval 6.0 to 8.5) in women not using hormonal contraception, 11.0 (9.6 to 12.6) in women using high risk hormonal contraception, 7.9 (5.9 to 10.6) in those using medium risk hormonal contraception, and 4.5 (2.6 to 8.1) in users of low/no risk hormonal contraception. The corresponding numbers of extra venous thromboembolic events per 100 000 women over the first week of NSAID treatment compared with non-use of NSAIDs were 4 (3 to 5) in women not using hormonal contraception, 23 (19 to 27) in women using high risk hormonal contraception, 11 (7 to 15) in those using medium risk hormonal contraception, and 3 (0 to 5) in users of low/no risk hormonal contraception.
Conclusions
NSAID use was positively associated with the development of venous thromboembolism in women of reproductive age. The number of extra venous thromboembolic events with NSAID use compared with non-use was significantly larger with concomitant use of high/medium risk hormonal contraception compared with concomitant use of low/no risk hormonal contraception. Women needing both hormonal contraception and regular use of NSAIDs should be advised accordingly.
The BMJ linked editorial – NSAIDs, hormonal contraception, and venous thromboembolism (Open access)
See more from MedicalBrief archives:
Contraception with fewer hormones still effective – Philippines modelling study
Link confirmed between the Pill and clot risk
Contraception with fewer hormones still effective – Philippines modelling study
NSAIDs link with cardiovascular events