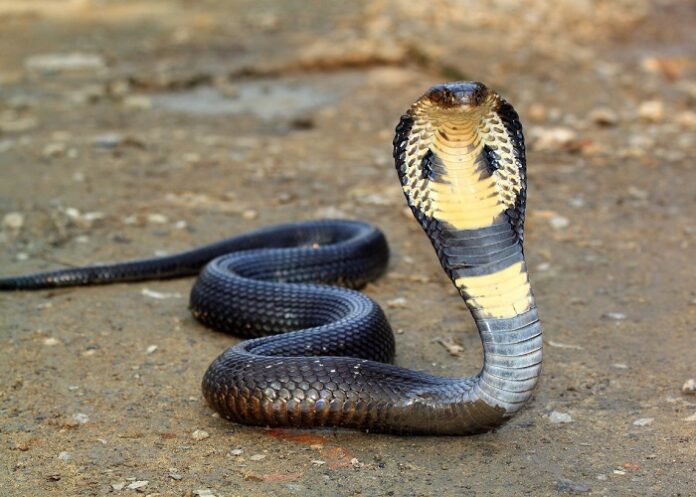
A commonly used blood thinner can be used as an antidote to cobra venom, an international study has suggested, research that experts have described as “really exciting” and which could help save lives.
Snakebite is considered a neglected tropical disease by the World Health Organisation, and although antibody-based anti-venoms exist, they are species specific, expensive and require cold storage as well as intravenous administration in a health care setting.
In this recent study, published in the Journal of Science Translational Medicine, Professor Nicholas Casewell from Britain’s Centre for Snakebite Research and Interventions at Liverpool School of Tropical Medicine, said snakebites were the “deadliest of neglected tropical diseases, with the burden landing overwhelmingly on rural communities in low and middle income countries”.
Cobra bites are usually treated using anti-venom administered through an intravenous drip, meaning the drug reaches the bloodstream rather than the tissue. Anti-venom treatments are therefore ineffective in treating necrosis, the irreversible death of body tissue, which can lead to amputation or a loss of limb function.
Treatment is also expensive, and it can take days for patients to get to a hospital, reports The Guardian.
The lead author of the study, Tian Du from the University of Sydney, said if human trials were successful, heparin – a blood thinner that can directly reach infected tissue – could be used on-site, most likely in combination with other drugs.
Du said after successful human trials, heparin, which is a WHO-listed essential medicine, could be rolled out relatively quickly to become a cheap, safe and effective drug for treating cobra bites.
While she said it was unclear at this stage how much heparin would reduce tissue damage, she was hopeful that damage would be reduced by 50% to 100%, depending on the dosage and how quickly the drug was delivered.
The WHO has announced a goal of halving the number of deaths and disability due to snakebites by 2030, having recognised these as a priority among neglected tropical diseases. While the number of people bitten by cobras is unclear, cobra species account for most snakebite incidents in parts of India and Africa.
The research team analysed which genes are targeted by snake venom. They then identified that these genes are responsible for producing heparan sulfate on the surface of cells, as well as heparin sulfate, which is released in an immune response. Heparin acts as a decoy antidote binding to and neutralising toxins within the venom which causes tissue damage
The researchers used the same method to find an antidote to box jellyfish venom in 2019, and are working on finding similar antidotes for Australian black snakes and blue bottle stings.
Associate Professor Bryan Fry, a venom expert at the University of Queensland who wasn’t involved in the study, said the research was “really exciting stuff”.
“Cobra venoms cause profound local tissue damage … it’s as if you’ve injected the person with acid,” he said. “This is the first study of its type with this particular toxin class and the action that it has.”
Study details
Molecular dissection of cobra venom highlights heparinoids as an antidote for spitting cobra envenoming
Tian Y. Du, Steven Hall, Felicity Chung, Nicholas Casewell et al.
Published in Journal of Science Translational Medicine on 17 July 2024
Abstract
Snakebites affect about 1.8m people annually. The current standard of care involves antibody-based anti-venoms, which can be difficult to access and are generally not effective against local tissue injury, the primary cause of morbidity. Here, we used a pooled whole-genome CRISPR knockout screen to define human genes that, when targeted, modify cell responses to spitting cobra venoms. A large portion of modifying genes that conferred resistance to venom cytotoxicity was found to control proteoglycan biosynthesis, including EXT1, B4GALT7, EXT2, EXTL3, XYLT2, NDST1, and SLC35B2, which we validated independently. This finding suggested heparinoids as possible inhibitors. Heparinoids prevented venom cytotoxicity through binding to three-finger cytotoxins, and the US Food and Drug Administration–approved heparinoid tinzaparin was found to reduce tissue damage in mice when given via a medically relevant route and dose. Overall, our systematic molecular dissection of cobra venom cytotoxicity provides insight into how we can better treat cobra snakebite envenoming.
See more from MedicalBrief archives:
Anti-venom failure leads to novel toxin immunology discovery
Snakebite: ‘The world’s biggest hidden health crisis’
Venomics: Developing new medicines out of ancient animal poisons
Broad-spectrum snake venom antidote developed