Every year, about 14m women lose so much blood during childbirth that they could die: about 70 000 do.
The condition – postpartum haemorrhage (PPH) – can be stopped if health workers realise in time that a new mother is bleeding too much and can act quickly, but until now, there’s not been a standard way of knowing when blood loss is getting dangerous and what needs to be done.
Fortunately, new recommendations from the World Health Organisation are changing that and saving lives, writes Isabella Ochieng for Bhekisisa, describing what she and her colleagues have experienced in their labour wards in Kenya.
At the Malindi Sub-County Hospital, in Kilifi county along the east coast of Kenya, necessity is the mother of invention.
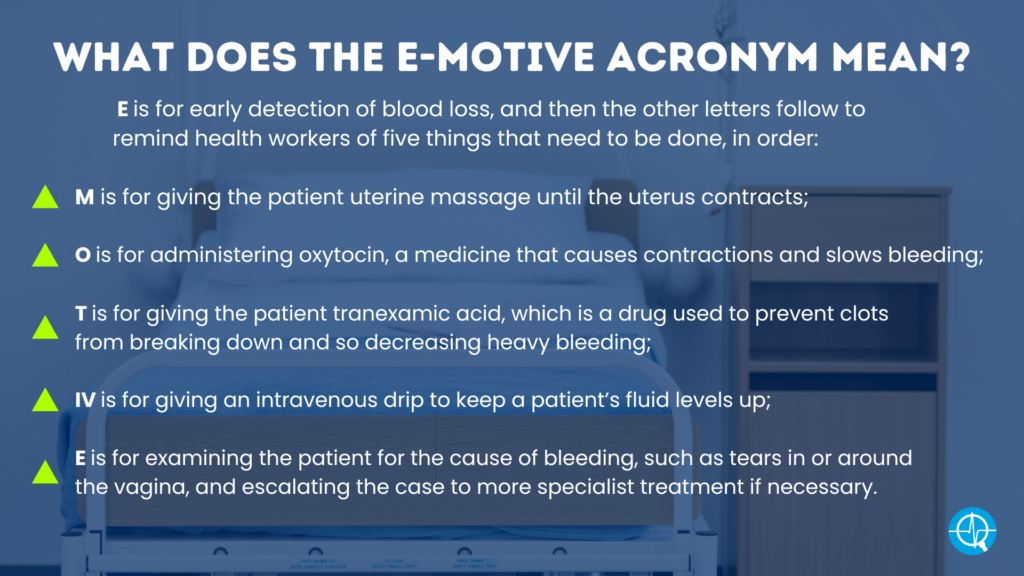
For three years, my colleagues and I participated in an international study evaluating a treatment approach called E-MOTIVE to help women who’ve just given birth from losing too much blood.
Losing more than half a litre of blood or more in 24 hours after giving birth (PPH) affects 14m women annually, with one dying every six minutes because of it. This is due to various contributing factors, one being that visual estimation of blood lost is known to be inaccurate.
Soon after learning how to implement the E-MOTIVE approach, we realised it was a lifesaver. Being able to accurately measure blood loss helps with diagnosing PPH in time.
The study showed that acting on the diagnosis reduced – by 60% – PPH, deaths or the need for surgery.
But when the trial ended, we stopped receiving the commodities that were needed to conduct the study. Not least were the imported blood-collecting drapes.
So my colleagues invented their own drape-like apron made from waterproof hospital mattress pads we had on hand in our hospital, and stitched by a local tailor, to funnel blood into a pan with calibrated markings.
This makeshift solution shows how much they believe in this management approach. In fact, they had wholeheartedly embraced it even before the results of the trial of the WHO’s first-response bundle for PPH were published.
The WHO has since also published recommendations for standardised guidelines so health workers know to identify PPH and how it should be treated. Further, the WHO says a clear plan for making the approach work must be available, such as training health staff where they work and having all the needed supplies on hand.
While each individual component of the E-MOTIVE treatment had previously been studied and recommended for women with PPH, the bundle approach, meaning doing the five things as a set, had not.
My role in the E-MOTIVE research project was to train colleagues on providing the care as a series, supervising them as they worked.
Scepticism from some, or resistance to doing things differently (for example, doing only one of the five things or choosing to refer the case to a doctor from the start) evaporated when we saw just how effective the bundle approach is when combined with early detection using the drapes.
Putting the approach into practice resulted in only two or three new mothers every week experiencing excessive blood loss in our labour ward, instead of the previous five or six.
The death of a mother has devastating consequences for her family and community. Research shows that newborns whose mothers died before they were six-months-old, for example, during childbirth, are five times more likely to die before they grow into adults than those whose mothers survive.
No more guesswork
Nurses, midwives and other health workers, as new mothers’ caregivers, also suffer when a patient dies.
It’s demoralising and draining to work tirelessly to keep women safe during childbirth yet still lose so many to a preventable condition like PPH.
Unlike patients who are clearly very ill, these young women often look well – they’re breastfeeding, smiling and joking.
Then suddenly, they’re in the throes of the life-threatening crisis of severe bleeding after birth. It’s chilling and shocking.
Midwives like us, who have first-hand experience of implementing the bundle, also feel newly empowered. We no longer need to summon doctors in a panic when a woman bleeds excessively. With the bundle, we can confidently and competently manage most cases.
And because we learned how to apply the approach, along with nurses and doctors, a respectful sense of teamwork emerged.
Doctors now seem less likely to demand that we defend our clinical judgment, and are less inclined to ask, “Why did you give tranexamic acid?”
In the past, this may have been a valid question by a doctor. We know now that giving women this drug in time to stop heavy bleeding is a crucial step of the treatment bundle.
While Kenyan health facilities may have this medicine on hand, it’s usually reserved for other purposes, like trauma cases, and not routinely used for management of PPH.
We know that the bundle works – but only when it’s started on time and all the supplies needed for it are available, including drapes and drugs like tranexamic acid.
Hospital administrators and procurement officers need to be made aware of what the E-MOTIVE bundle can mean for keeping women safe during childbirth, as should Health Ministries, which have the power to update policy recommendations.
If all of my colleagues were trained to implement the bundle and have all the necessary commodities, I think my country could reduce severe PPH by even more than 60% – maybe as much as 80%.
Ochieng, a nurse midwife and maternal and newborn health technical adviser for Jhpiego, worked on the E-MOTIVE trial.
Study details
Randomised Trial of Early Detection and Treatment of Postpartum Haemorrhage
Ioannis Gallos, James Martin, Lumaan Sheikh, et al.
Published in The New England Journal of Medicine on 6 July 2023
Abstract
Background
Delays in the detection or treatment of postpartum haemorrhage can result in complications or death. A blood-collection drape can help provide objective, accurate, and early diagnosis of postpartum haemorrhage, and delayed or inconsistent use of effective interventions may be able to be addressed by a treatment bundle.
Methods
We conducted an international, cluster-randomised trial to assess a multicomponent clinical intervention for postpartum haemorrhage in patients having vaginal delivery. The intervention included a calibrated blood-collection drape for early detection of postpartum haemorrhage and a bundle of first-response treatments (uterine massage, oxytocic drugs, tranexamic acid, intravenous fluids, examination, and escalation), supported by an implementation strategy (intervention group). Hospitals in the control group provided usual care. The primary outcome was a composite of severe postpartum haemorrhage (blood loss, ≥1000 ml), laparotomy for bleeding, or maternal death from bleeding. Key secondary implementation outcomes were the detection of postpartum haemorrhage and adherence to the treatment bundle.
Results
A total of 80 secondary-level hospitals across Kenya, Nigeria, South Africa, and Tanzania, in which 210,132 patients underwent vaginal delivery, were randomly assigned to the intervention group or the usual-care group. Among hospitals and patients with data, a primary-outcome event occurred in 1.6% of the patients in the intervention group, as compared with 4.3% of those in the usual-care group (risk ratio, 0.40; 95% confidence interval [CI], 0.32 to 0.50; P<0.001). Postpartum haemorrhage was detected in 93.1% of the patients in the intervention group and in 51.1% of those in the usual-care group (rate ratio, 1.58; 95% CI, 1.41 to 1.76), and the treatment bundle was used in 91.2% and 19.4%, respectively (rate ratio, 4.94; 95% CI, 3.88 to 6.28).
Conclusions
Early detection of postpartum haemorrhage and use of bundled treatment led to a lower risk of the primary outcome, a composite of severe postpartum haemorrhage, laparotomy for bleeding, or death from bleeding, than usual care among patients having vaginal delivery.
See more from MedicalBrief archives:
African study finds solution to reduce for childbirth-related haemorrhaging
Cochrane Review identifies alternative drugs better to prevent PPH
Tranexamic acid decreasing death risk from post-partum blood loss
Cooling cuts post partum blood loss
