Some men with advanced prostate cancer who have exhausted all other treatment options could live for two years or more on immunotherapy, a major clinical trial has shown. Researchers found that a small proportion of men were ‘super responders’ and were alive and well even after the trial had ended despite having had a very poor prognosis before treatment.
The study found that one in 20 men with end-stage prostate cancer responded to the immunotherapy pembrolizumab – but although the number who benefited was small, these patients sometimes gained years of extra life.
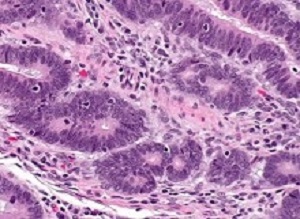
The most dramatic responses came in patients whose tumours had mutations in genes involved in repairing DNA, and the researchers are investigating whether this group might especially benefit from immunotherapy.
The phase II clinical trial, called KEYNOTE-199, was led globally by a team at The Institute of Cancer Research, London, and The Royal Marsden NHS Foundation Trust, and involved 258 men with advanced prostate cancer who had previously been treated and become resistant to androgen deprivation therapy and docetaxel chemotherapy. The study was funded by the drug’s manufacturer Merck known as MSD outside the US and Canada.
Overall, 5% of men treated with pembrolizumab saw their tumours actually shrink or disappear, while a larger group of 19% had some evidence of tumour response with a decrease in prostate-specific antigen (PSA) level. Among a group of 166 patients with particularly advanced disease and high levels of PSA, the average length of survival was 8.1 months with pembrolizumab.
Nine of these patients saw their disease disappear or partly disappear on scans. And of these, four were super-responders who remained on treatment at the end of study follow-up, with responses lasting for at least 22 months.
A second group of patients whose PSA levels were lower but whose disease had spread to the bone lived for an average of 14.1 months on pembrolizumab.
New larger trials are now under way to test whether men with DNA repair gene mutations in their tumours, or those whose cancer has spread to the bone, should receive pembrolizumab as part of their care.
The study also compared the effectiveness of pembrolizumab in men whose tumours had a protein called PD-L1 on the surface of their cancer cells and those whose tumours did not. Targeting PD-L1 activity with pembrolizumab takes the ‘brakes’ off the immune system, setting it free to attack cancer cells.
But the study found that testing for PD-L1 was not sufficient to tell which patients would respond to treatment. Men with PD-L1 in their tumours survived 9.5 months compared with 7.9 months for patients without PD-L1 in their tumours.
Identifying better tests to pick out who will respond best will be critical if pembrolizumab is to become a standard part of prostate cancer treatment. Pembrolizumab was well tolerated, with 60% of patients reporting any side effects and only 15% of patients experiencing grade 3-5 side effects.
Professor Johann de Bono, Regius professor of cancer research at The Institute of Cancer Research, London, and consultant medical oncologist at The Royal Marsden NHS Foundation Trust, said: “Our study has shown that a small proportion of men with very advanced prostate cancer are super responders to immunotherapy and could live for at least two years and possibly considerably longer.
“We don’t see much activity from the immune system in prostate tumours, so many oncologists thought immunotherapy wouldn’t work for this cancer type. But our study shows that a small proportion of men with end-stage cancer do respond, and crucially that some of these men do very well indeed.
“We found that men with mutations in DNA repair genes respond especially well to immunotherapy, including two of my own patients who have now been on the drug for more than two years. I am now leading a larger-scale trial specifically for this group of patients and am excited to see the results.”
Professor Paul Workman, CEO of The Institute of Cancer Research, London, said: “Immunotherapy has had tremendous benefits for some cancer patients and it’s fantastic news that even in prostate cancer, where we don’t see much immune activity, a proportion of men are responding well to treatment.
“A limitation with immunotherapy is that there’s no good test to pick out those who are most likely to respond. It’s encouraging to see testing for DNA repair mutations may identify some patients who are more likely to respond, and I’m keen to see how the new, larger trial in this group of patients plays out.”
Abstract
Purpose: Pembrolizumab has previously shown antitumor activity against programmed death ligand 1 (PD-L1)–positive metastatic castration-resistant prostate cancer (mCRPC). Here, we assessed the antitumor activity and safety of pembrolizumab in three parallel cohorts of a larger mCRPC population.
Methods: The phase II KEYNOTE-199 study included three cohorts of patients with mCRPC treated with docetaxel and one or more targeted endocrine therapies. Cohorts 1 and 2 enrolled patients with RECIST-measurable PD-L1–positive and PD-L1–negative disease, respectively. Cohort 3 enrolled patients with bone-predominant disease, regardless of PD-L1 expression. All patients received pembrolizumab 200 mg every 3 weeks for up to 35 cycles. The primary end point was objective response rate per RECIST v1.1 assessed by central review in cohorts 1 and 2. Secondary end points included disease control rate, duration of response, overall survival (OS), and safety.
Results: Two hundred fifty-eight patients were enrolled: 133 in cohort 1, 66 in cohort 2, and 59 in cohort 3. Objective response rate was 5% (95% CI, 2% to 11%) in cohort 1 and 3% (95% CI, < 1% to 11%) in cohort 2. Median duration of response was not reached (range, 1.9 to ≥ 21.8 months) and 10.6 months (range, 4.4 to 16.8 months), respectively. Disease control rate was 10% in cohort 1, 9% in cohort 2, and 22% in cohort 3. Median OS was 9.5 months in cohort 1, 7.9 months in cohort 2, and 14.1 months in cohort 3. Treatment-related adverse events occurred in 60% of patients, were of grade 3 to 5 severity in 15%, and led to discontinuation of treatment in 5%.
Conclusion: Pembrolizumab monotherapy shows antitumor activity with an acceptable safety profile in a subset of patients with RECIST-measurable and bone-predominant mCRPC previously treated with docetaxel and targeted endocrine therapy. Observed responses seem to be durable, and OS estimates are encouraging.
Authors
Emmanuel S Antonarakis; Josep M Piulats; Marine Gross-Goupil; Jeffrey Goh; Kristiina Ojamaa; Christopher J Hoimes; Ulka Vaishampayan; Ranaan Berger; Ahmet Sezer; Tuomo Alanko; Ronald de Wit; Chunde Li; Aurelius Omlin; Giuseppe Procopio; Satoshi Fukasawa; Ken-ichi Tabata; Se Hoon Park; Susan Feyerabend; Charles G. Drake; Haiyan Wu; Ping Qiu; Jeri Kim; Christian Poehlein; Johann Sebastian de Bono
[link url="https://www.icr.ac.uk/news-archive/prostate-cancer-super-responders-live-for-two-years-on-immunotherapy"]The Institute of Cancer Research material[/link]
[link url="https://ascopubs.org/doi/10.1200/JCO.19.01638"]Journal of Clinical Oncology abstract[/link]