 The Prolift vaginal mesh implant was launched despite the company being warned it could shrink and harden inside the body, according to an international investigation into medical devices, reported in The Guardian. And DePuy is bearing the UK National Health Service's costs of caring for patients given its defective hip replacements.
The Prolift vaginal mesh implant was launched despite the company being warned it could shrink and harden inside the body, according to an international investigation into medical devices, reported in The Guardian. And DePuy is bearing the UK National Health Service's costs of caring for patients given its defective hip replacements.
Internal emails between executives show staff at Johnson & Johnson (J&J) were concerned that the plastic material the mesh was made from had the potential to turn “hard as a rock” and roll up like a “folded potato chip” inside patients.
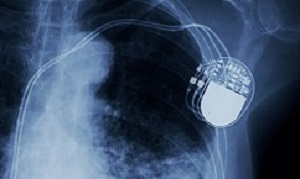
Patients around the world are suffering pain and many have died as a result of faulty medical devices that have been allowed on to the market by a system dogged by poor regulation, lax rules on testing and a lack of transparency, The Guardian reports an investigation has found. Pacemakers, artificial hips, contraceptives and breast implants are among the devices that have caused injuries and resulted in patients having to undergo follow-up operations or in some cases losing their lives. In some cases, the implants had not been tested in patients before being allowed on to the market.
The report says patients around the world are suffering pain and many have died as a result of faulty medical devices that have been allowed on to the market by a system dogged by poor regulation, lax rules on testing and a lack of transparency, an investigation has found.
Pacemakers, artificial hips, contraceptives and breast implants are among the devices that have caused injuries and resulted in patients having to undergo follow-up operations or in some cases losing their lives. In some cases, the implants had not been tested in patients before being allowed on to the market.
The report says in the UK alone, regulators received 62,000 “adverse incident” reports linked to medical devices between 2015 and 2018. A third of the incidents had serious repercussions for the patient, and 1,004 resulted in death. In the US, the Food and Drug Administration (FDA) has collected 5.4m “adverse event” reports over the past decade, some from manufacturers reporting problems in other parts of the world. These included 1.7m reports of injuries and almost 83,000 deaths. Nearly 500,000 mentioned an explant – surgery to remove a device.
The report says the figures come from research by 252 journalists from 59 media organisations in 36 countries, which has uncovered a litany of problems in the global $400bn industry.
Examples of failure in the market include: replacement hips and vaginal mesh products sold to hospitals without any clinical trials; patients relying on faulty pacemakers when manufacturers were aware of problems; complications with hernia mesh that ruled one of Britain’s top athletes out of competing for years; regulators approving spinal disc replacements that later disintegrated and migrated in patients; surgeons admitting they were unable to tell patients about the risks posed by implants because of a lack of central registers; and patients in Australia being given devices that the regulator has approved on the basis they have been approved in Europe.
The report says the findings raise concerns about the level of scrutiny devices undergo before and after they go on the market, and whether regulators detect and act upon findings quickly enough.
Information about problems with devices is, in many countries, kept under wraps, making it difficult for patients to research procedures that have been recommended to them.
Professor Derek Alderson, the president of the Royal College of Surgeons, said there had been enough incidents involving flawed devices to “underline the need for drastic regulatory changes”, including the introduction of mandatory national registries for all implantable devices. “In contrast to drugs, many surgical innovations are introduced without clinical trial data or centrally held evidence,” he said. “This is a risk to patient safety and public confidence.”
The report says journalists, coordinated by the International Consortium of Investigative Journalists (ICIJ), have trawled through thousands of documents, many obtained through freedom of information (FoI) requests, to unearth some of the biggest problems. Alongside interviews with patients and doctors, these have revealed flaws in the way the industry is regulated that are unlikely to be fixed by rules due to come into force in Europe.
Among the concerns raised by the Implant Files project are that manufacturers are in charge of testing their own products after faults have developed – and are allowed to shop around for approval to market their products, without declaring any refusals. Doctors were also found to have close industry ties or seem eager to be early adopters of the latest devices to enhance their professional standing.
Plans for tougher EU rules have been watered down after industry lobbying, according to a huge trove of documents uncovered by the project. Dagmar Roth-Behrendt, the German MEP who led the EU’s move to overhaul medical device regulation, is quoted in the report as saying lobbying by the industry and trade associations was “the blackest I’ve seen”. She said: “I’ve seen a huge amount of (lobbying) in the 25 years I was in the European parliament (on) internal market legislation on food and on many other things – on cars, on tobacco, on whatever.”
In the UK, an FoI request sent to the Medicines and Healthcare Products Regulatory Agency (MHRA) revealed it had received an adverse incident report on average every half an hour over the past three years. The reports related to a huge range of products including wheelchairs, beds and catheters as well as implants. Vaginal mesh, hip and knee replacements were among devices associated with thousands of the reports.
The MHRA passes all its reports on to manufacturers and in some cases sets up a serious investigation, led by its experts. But, the report says, data from FoI requests shows there has been a collapse in the proportion of investigations overseen by the MHRA at a time when complaints are soaring. So far in 2018, one in 100 reports received have prompted it to start a special investigation, compared with one in three in 2008. Instead, the majority of reports have been passed on to manufacturers and fed into the regulator’s “trending and surveillance” database.
Graeme Tunbridge, the group manager for devices regulatory affairs at the MHRA, said in the report that the fall in the number of investigations reflected a change in the way it worked. “We have been moving towards a more sophisticated and trend-led approach. Most problems are systems-level issues, not unique to a single instance, for example where a whole batch is manufactured with a defect. Grouping incidents allows us to see the bigger picture and find the true causes of issues and solve them.”
The MHRA said reports received via its “yellow card” online reporting system did not necessarily mean there was a fault with a device, and that an adverse incident may be the result of a pre-existing medical condition, or the device may not have been used as intended.
The report says rules making it tougher for devices to get approval are due to be introduced in Europe in 2020. Tunbridge said the MHRA had been instrumental in agreeing the new legislation, and that it would strengthen the regulatory framework. “Our highest priority is making sure the medical devices available in the UK work and are acceptably safe,” he said.
But critics remain sceptical. The report says most devices are cleared through a pathway that allows new products to inherit the approval status of “substantially equivalent” ones that are already on the market, without the need for further trials.
In some cases, after lengthy chains of equivalence-based approvals, new devices scarcely resemble the original version, which may have been withdrawn from use. A British Medical Journal study last year traced the family tree of 61 surgical mesh products to two original devices approved in 1985 and 1996.
Carl Heneghan, a professor of evidence-based medicine at the University of Oxford, said systemic failings in the way medical implants were regulated meant “patients are in one big experiment and they often don’t know it”. He said in the report that the rules due to be introduced in Europe would not fix the structural problems. “You can’t see the evidence that a device is built on – that’s still the same,” he said. “It’s still commercial organisations that control the flow of data.”
Other FoI requests made to the MHRA underline how difficult it is to get information on what is going wrong with devices. The report says details were requested of incidents relating to the contraceptive Essure, but the request was turned down on the basis of commercial confidentiality. Such a response is not unusual, according to a recent paper by scientists.
One of the biggest medical companies in the world has, meanwhile, admitted it is having to pay out to the UK’s National Health Service (NHS) to cover the cost of monitoring and operating on patients who were given defective hip replacements. The Guardian reports that DePuy, owned by Johnson & Johnson, would not say how much it had handed over, but it could run into millions. It recalled a metal-on-metal hip system in 2010 after it emerged that debris from wear and tear was causing damage and resulting in a large number of surgical revisions.
The report says the company withdrew the products – a range known as the ASR (articular surface replacement) system – and advised that patients should have tests to check cobalt and chromium ion levels in their blood and, in some cases, MRI scans or X-rays. Many patients have had follow-up operations to remove the defective hips and replace them, and the NHS is continuing to monitor others.
Johnson & Johnson is quoted in the report as saying it had made payments towards the costs. A spokesperson said: “Under the ASR hip system reimbursement programme … DePuy Synthes has provided reimbursement to the NHS trusts and other healthcare providers for applicable testing and treatment, including expenses related to revision surgeries.”
The ASR system was approved for use in Europe in 2003, but was not used by the NHS until the following year. By the time it was withdrawn it had been used in about 10,000 patients. The report says when approved by European regulators it had not been tested in humans, but had been subject to extensive laboratory and simulator tests.
While many replacement hips performed well, problems emerged with two new procedures that involved metal parts. One procedure involved a total hip replacement, whereby a metal ball and stem were attached to the thigh bone, and a metal cup attached to the pelvis. The other was the hip resurfacing system. For this, the ball of a patient’s hip joint was retained, but a metal cap was put over its surface. This then sat within another metal cap on the pelvis.
The report says in the UK, Midland Medical Technologies (MMT) was the first to bring this procedure to the market with its Birmingham Hip Resurfacing (BHR) system, which was launched in 1997. MMT was bought by the UK medical equipment firm Smith & Nephew in 2004 for £67m.
After the success of this implant, DePuy brought its own version to the market in 2003. Its metal-on-metal resurfacing won approval in Europe on the basis of laboratory testing, including the use of simulators, rather than through clinical trials on people.
One retired hip surgeon, who did not use the ASR system, said people would visit his clinic asking for the treatment after hearing about it from friends or adverts. “At the time, I think we were all amazed how quickly the ASR and large head metal-on-metal hip replacement was taken up throughout the UK and in fact around the world,” said Keith Tucker, a retired surgeon who is chair of the Orthopaedic Data Evaluation Panel. “Resurfacing seemed to have become very fashionable and often the demand was driven by patients who had heard about it from various sources.”
But, the report says, in 2007 the Australian Orthopaedic Association national joint replacement registry noted that ASR seemed to have twice the risk of revision – the need for further surgery – compared with other resurfacing procedures. The following year, the registry published data showing some women undergoing metal-on-metal hip resurfacing were facing more follow-up operations than others.
In 2010, DePuy withdrew its implants after the National Joint Registry (NJR) for England and Wales shared data showing higher than expected revision rates among patients with metal-on-metal hips. Within five years of receiving DePuy’s resurfacing device, 12% of patients had undergone revision surgery, and within five years of having an ASR total hip replacement the figure was 13%.
DePuy’s spokesperson said the company had carefully analysed the data from Australia and communicated with surgeons about which patients should receive the ASR hips. “DePuy constantly reviewed and evaluated surveillance data concerning the ASR hip system from a variety of sources, including national joint replacement registries, internal complaints data, peer-reviewed published literature, company-sponsored clinical trials, and external clinical research reports, as we do with all of our products,” the spokesperson said.
“Until August 2010, when DePuy announced the voluntary recall, the totality of the data available to DePuy indicated that the revision rate of the ASR hip system was similar to that reported for other large diameter metal-on-metal monoblock and resurfacing hip devices.”
The report says in the years that followed, other manufacturers withdrew from the market as more data showed the high level of follow-up surgery needed by patients.
In 2015, Smith & Nephew advised that its BHR system should not be used in females or in men needing the smaller-sized implants. A spokesperson for the company said the data did not indicate there was a single, dominant reason why the revision rate was higher in these patients. “For instance, in various registries, there are a range of fairly typical diagnoses, including infection, dislocation, metal sensitivity, loosening/lysis and fracture,” the spokesperson said.
In the US, patients who have faced further surgery as a result of problems with metal-on-metal hips have been awarded damages, but in the UK there has not been a successful court case. The report says this year, a UK judge found against patients who were seeking compensation from DePuy after experiencing problems with a different metal-on-metal hip it made. The patients’ lawyers claimed high revision rates recorded in the NJR were a sign of problems with the product.
However, DePuy argued the issues were a result of a “nocebo effect”, where patients who had seen that the hip had been recalled had experienced problems as a result of their negative expectations of the implants. Several other cases against manufacturers are in the balance as lawyers work out if there is any chance of them succeeding.
Tim Annett, a partner at the law firm Irwin Mitchell, said in the report that the bar had been set very high by the High Court. “You would have to show that the risk is significantly higher from these hips (than for other hips), and possibly double, although this was not confirmed by the ruling.”
A vaginal mesh implant made by one of the world’s biggest pharmaceutical firms was launched despite the company being warned it could shrink and harden inside the body. The Guardian reports that internal emails between executives show staff at Johnson & Johnson (J&J) were concerned that the plastic material the mesh was made from had the potential to turn “hard as a rock” and roll up like a “folded potato chip” inside patients.
Despite this risk, the Prolift implant was made available in 2005 and marketed for seven years. In one exchange, staff discussed how “shrinkage of the mesh may lead to pain”.
The report says the documents are among hundreds submitted to a US court as part of a civil case brought by Suzanne Emmett, 60, from Pennsylvania. She is one of many women who allege they suffered traumatic complications after receiving the implant. Emmett is suing J&J for damages, and a Philadelphia court will hear this week that she needed nine revision surgeries and has been left struggling to cope with her pain after the implant perforated her vagina. J&J is contesting the claims.
Emmett’s legal team alleges the mesh device was defective and the company was negligent in its manufacture and failed to warn doctors of all the potential dangers.
The report says the Prolift was designed to treat pelvic organ prolapse, in which the muscles supporting the pelvic organs weaken and one or more of them press into the vagina, sometimes causing discomfort. It was launched in the US in 2005 without approval from the Food and Drug Administration (FDA) and only obtained clearance three years later after the US regulator was alerted it was on the market.
The report says at the time, J&J argued the implants were sufficiently similar to existing products that it believed approval was not required. The company said it could not confirm whether the implant had CE mark safety approval in Europe “due to ongoing litigation”.
Emmett was given the implant in 2007. She says that, several months later, the mesh had cut through into her vagina and since then has resurfaced more than a dozen times, with surgeons removing it piece by piece. Her husband’s penis was scratched by the mesh during sex, which he likened to “barbed wire”. Emmett says she suffers painful bladder contractions, urge incontinence and that her sex life has been affected.
Company documents provided to the court as part of the case show J&J was keen to position Prolift as a more effective alternative to traditional surgery, which has a recurrence rate of about 30%. However, the report says ahead of its launch, J&J staff also discussed the implant’s potential downsides. In a message dated May 2004, a product director at J&J’s Ethicon unit, which sold the implants, warned of the potential for the mesh to harden and fold.
The company received correspondence from surgeons raising concerns. In a 2005 message, months after the device was launched, Professor Linda Cardozo, from King’s College Hospital in London, told a senior J&J manager that she found Prolift’s safety profile “quite worrying” and doctors had been given “no efficacy data to review”. “I still have major concerns regarding the erosion rate and possible problems with (sex becoming painful),” she wrote. Cardozo said she subsequently remained unconvinced by Prolift and had not used it.
The report says the paperwork provided to the court also included details of a study of 90 women who were given the implants between 2004 and 2006 and followed up for a year. Doctors reported an 18% failure rate, the mesh had eroded into the vagina in 9% of women and 13% had “moderate or severe vaginal retraction”, where the tissue hardens and contracts due to scarring around the implant.
The mesh implants, which are designed to be permanent, become embedded in the pelvic tissue. If the material shrinks, nerves in the tissue can be compressed, causing pain.
The court documents suggest that J&J executives liaised with US doctors behind the scenes about lobbying. The report says one email chain discussed how to mount an offensive after the American College of Obstetricians and Gynaecologists (ACOG) warned its 55,000 members in February 2007 that mesh implants should be viewed as “experimental”.
Dr Vincent Lucente, a US doctor who was paid $1.7m by the company over 12 years in travel expenses, consulting and training fees, advised J&J executives to launch a “great offence” to get the guidance changed. “I suggest a physician leader with whom you can work with be a female, well respected, with no strong industry ties,” he wrote in a 2007 email.
By September 2007, ACOG had replaced the bulletin with an updated version, without the word “experimental”, which Lucente said was down to his efforts. A J&J marketing director responded: “I am doing the happy dance! I love you man!”
ACOG said the change had been made after it received emails, letters and phone calls from members who objected to the use of the word “experimental, which these members felt did not “accurately reflect the expanding use of these surgical approaches”. Lucente did not play any role in the revision, it said.
Lucente is quoted in the report as saying he had made a single phone call to ACOG because he believed the bulletin was “factually incorrect”. “There was no lobbying; it definitely wasn’t done on behalf of Ethicon or any other industry,” he said.
In 2017, the UK’s National Institute for Health and Care Excellence guidelines recommended that mesh should no longer be used to treat prolapse. In June 2012, J& J voluntarily withdrew Prolift from the market, after being ordered by the FDA to carry out further testing.
The report says asked about the issues raised by the documents, J&J declined to comment. In a statement, the company said: “We think it is inappropriate to litigate these issues in the media or for conclusions to be drawn based on references to selectively chosen documents taken out of context.”
[link url="https://www.theguardian.com/society/2018/nov/25/revealed-faulty-medical-implants-harm-patients-around-world"]The Guardian report[/link]
[link url="https://www.icij.org/investigations/implant-files/"]Implant Files project[/link]
[link url="https://bmjopen.bmj.com/content/7/12/e017125"]BMJ abstract[/link]
[link url="https://www.theguardian.com/society/2018/nov/26/firm-pays-out-nhs-defective-hip-replacements?CMP=Share_iOSApp_Other"]The Guardian report[/link]
[link url="https://www.theguardian.com/society/2018/nov/27/vaginal-mesh-implant-sold-despite-warnings-could-cause-pain-johnson-johnson"]The Guardian report[/link]
