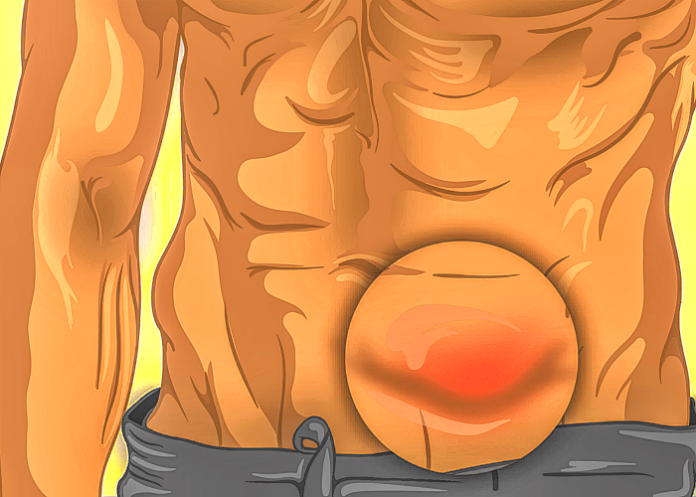
Hernia repair is one of the most common operations performed and is widely viewed as a simple procedure carrying minimal risk, writes MedicalBrief. Yet in the US, one-in-six procedures require a re-operation within 10 years and hernia recurrence has been reported to be as high as 60%, notes an analysis in JAMA Network.
The repeat hernia surgery rates have barely improved since the 1990s, when similar data revealed that about one in five patients underwent at least two surgeries to address the problem, writes Dr Ryan Howard, general surgery resident at Michigan Medicine, who is also involved with research for the Michigan Surgical Quality Collaborative Hernia Registry, in a research letter.
Hernia repair is one of the most common operations performed in the US. Each year, more than 350,000 patients undergo ventral and incisional hernia repair and more than 800,000 undergo inguinal hernia repair.
Howard and colleagues conducted large analysis of hernia recurrence across a national population. In a cohort of nearly 200,000 older US adults, they found that one in every six patients who underwent ventral hernia repair went on to have at least one more operation for hernia recurrence within 10 years. Importantly, because the study only measured how many patients had surgery for hernia recurrence, Howard writes, “we almost certainly underestimated the true incidence of recurrence. Not all patients who have a recurrence choose or are candidates for additional surgery. In fact, at least one study suggests that re-operation underestimates true recurrence by four-fold.”
In contrast, complication rates have reached impressively low levels for other common operation, like cholecystectomy and hysterectomy. Current safe cholecystectomy initiatives are working to even further decrease a bile duct injury rate that currently sits around 0.3%, writes Howard.
Complications related to quality of life continue to be common. Hernia recurrence – the risk of the hernia coming back after surgery to fix it – has been reported to be as high as 60%.
Equally concerning, compared with a similar study from 2003 that found one in five patients underwent re-operation within 10 years, the current results suggest that even 20 years later, outcomes after this extremely common operation have only marginally improved.
In Medpage Today, Howard writes that hernia repair is generally thought of as a common operation, “a simple, straightforward procedure that carries minimal risk and that virtually any surgeon can perform safely” . Put another way, many see it as “just a hernia”.
In this context, it is crucial to redouble research efforts to understand the drivers of these outcomes and how to improve them. Ventral hernia is a common problem that makes up a large proportion of annual surgical volume and is associated with billions in healthcare spending every year. However, compared with other common conditions, “scant federal clinical research dollars have been awarded to ventral hernia-associated investigation”.
If patient outcomes for this common operation are going to be improved, more research, and nuanced research, is needed. One of the most obvious ways to continue pushing research forward in this realm is to capture the heterogeneity that exists in hernia management, writes Howard.
“Hernias come in all shapes and sizes, but in many databases, a patient with a small port site hernia and a patient with a massive infected incisional hernia both get coded as ‘ventral hernia’. Therefore, accurately capturing this heterogeneity is paramount to improving hernia management. A number of efforts in the US are already doing precisely this.
The Abdominal Core Health Quality Collaborative maintains a national registry of surgeon-entered, voluntarily submitted hernia repairs that include fundamental characteristics such as hernia size, hernia location, mesh type, and a number of patient characteristics such as body mass index, smoking status, and diagnosis of diabetes, all of which are intimately related to hernia outcomes.
To further expand these efforts beyond voluntarily submitted cases, the Michigan Surgical Quality Collaborative Hernia Registry (MSQC-HR) was launched in 2020 to capture clinically rich hernia data at a population level. Akin to European hernia registries, the MSQC-HR will enable large-scale hernia research, but with the nuance necessary to meaningfully inform and improve practice. By capturing granular details regarding hernia size, location, mesh characteristics, and other critical factors, these efforts will help us understand the trajectory and outcomes of patients in the context of their hernia.
Already, this effort has revealed striking variation in mesh use, operative approach, patient selection, and short-term outcomes like complications, which suggests there is ample room for evidence-based practice standardisation and improvement, writes Howard.
“Finally, it will be critical to augment these results with long-term clinical and patient-reported outcomes. As we found in our recent study, a patient’s trajectory after ventral hernia repair plays out over years, not weeks.
“Longitudinal follow-up regarding patients’ quality of life, functional limitations, clinical and operative hernia recurrence, and long-term complications like chronic pain and infection, are needed to understand the full picture. To the extent that many of the outcomes after ventral hernia unfold more like chronic conditions than acute postoperative events, we must make routine collection of these conditions standard. Only then can we start to understand how changing something we do in the operating room can ensure the best possible result 5, 10, or even 20 years later, Howard writes.
Study details
Reoperation for Recurrence Up to 10 Years After Hernia Repair
Ryan Howard, Jyothi Thumma, Anne Ehlers, et al
Published in JAMA Network Open on 1 March 2022
Hernia recurrence following ventral or incisional hernia repair is a serious outcome that can occur years after surgery. Many studies of hernia recurrence are limited to short-term outcomes at single centers. The last study to characterise hernia recurrence at 10 or more years in a large US population was conducted from 1987 to 1999 and found a 20% rate of reoperation for recurrence at 10 years. We sought to characterise the long-term incidence of operative hernia recurrence up to 10 years after surgery in a contemporary US population of older adults.
Methods
We performed a retrospective review of 100% fee-for-service Medicare claims data to identify adult patients undergoing elective, inpatient, ventral or incisional and umbilical hernia repair from January 1, 2007, to December 31, 2018, using appropriate International Classification of Diseases, Ninth Revision (ICD-9) or International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) and Current Procedural Terminology (CPT) procedure codes with a corresponding ICD-9 or ICD-10 diagnosis code for the relevant type of hernia.
The primary outcome was reoperation for hernia recurrence, defined using the same ICD-9 or ICD-10 and CPT codes used to identify the index operation, as well as codes specific to recurrent hernia repair. Reoperation was identified during the follow-up period up to 10 years after the index hernia repair using patients’ unique Medicare Beneficiary Identifier.
A Cox proportional hazards model was used to calculate the cumulative incidence of hernia recurrence while adjusting for patient age, sex, race and ethnicity, 29 Elixhauser comorbidities, hernia type (ventral or incisional vs umbilical), and surgical approach (open vs minimally invasive). Patients were censored if they died, disenrolled from Medicare, or reached the end of the study period. Analyses were performed using Stata version 15.1 (StataCorp). No covariates were missing. This study of deidentified patient data was exempted from regulation by the University of Michigan Institutional Review Board and the need for informed consent was waived.
Results
Of the 175,735 patients who had undergone hernia repair, 162,292 underwent ventral or incisional hernia repair and 13,443 underwent umbilical hernia repair. The mean age was 68.9 years (SD, 11.1 years); 68,943 patients (39.2%) were men; 808 (0.5%) were Asian, 14, 235 (8.1%) were black, 3,348 (1.9%) were Hispanic, 1,102 (0.6%) were North American Native, 153,148 (87.2%) were white, 1,852 (1.1%) were of other race or ethnicity, and 1,242 (0.7%) were of unknown race or ethnicity. A total of 35,327 patients (20.1%) had a diagnosis of obesity at the time of index hernia repair. Median follow-up time was 5.3 years (IQR, 1.9-8.7 years).
A total of 25,061 patients (14.3%) underwent reoperation for hernia recurrence. The adjusted cumulative incidence of reoperation for recurrence was 16.1% (95% CI, 16.1%-16.2%) at 10 years after the index operation Among patients who underwent ventral or incisional hernia repair, the 10-year adjusted cumulative incidence of reoperation for recurrence was 16.0% (95% CI, 15.9%-16.0%) after open repair and 18.8% (95% CI, 18.7%-18.8%) following minimally invasive repair. Among patients who underwent umbilical hernia repair, the 10-year adjusted cumulative incidence of reoperation for recurrence was 12.3% (95% CI, 12.2%-12.3%) after open repair and 14.5% (95% CI, 14.5%-14.6%) following minimally invasive repair.
MedPage Today article – It’s not just a hernia (Second opinion) (Restricted access)
See more from MedicalBrief archives:
UK nurses to perform surgical procedures after 2-year training
Donations plea to fund Groote Schuur’s 6,000 surgery patients’ backlog
COVID-19 patients undergoing surgery at increased risk of post-operative death — NIHR
Relaxing of NHS targets on non-urgent surgery condemned
Nelson Mandela Bay surgeon sued over procedure 6 years ago