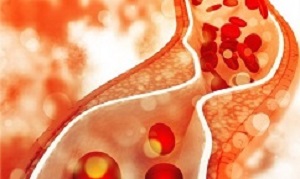
Adults as young as 25, not only older people, need to know their “bad cholesterol” (non-HDL) levels so they can change their lifestyle or take drugs to protect themselves against heart attacks and strokes in later life. The landmark study, involving data from nearly 400,000 people in 19 countries, establishes for the first time that levels of non-HDL are closely linked to the risk of heart disease across the entire life course.
The Guardian reports that a landmark study involving data from nearly 400,000 people in 19 countries has established for the first time that levels of non-HDL, or “bad cholesterol”, in the blood are closely linked to the risk of heart disease across the entire life course.
The research could lead to many younger people taking statins to lower their cholesterol levels. At the moment GPs prescribe the cholesterol-lowering drugs mostly to people in middle age. The authors said it was important to know your “bad” cholesterol level from young adulthood; it gave you the chance to lower the level through exercise, a healthier diet, or by taking statins.
“We need to start it early,” said Stefan Blankenberg, a professor in Hamburg, Germany, who was part of the multinational cardiovascular risk consortium that carried out the modelling study. He said would he like to see new guidance for doctors. “We should at least put into the guidelines that non-HDL cholesterol determination should be an obligation. At a very young age – 25 to 30. You need to know it.
He added: “In German schools we have large anti-smoking programmes. We persuade populations not to smoke. We have no programme to let people know about cholesterol. The first thing I would do is establish a cholesterol knowledge programme.” For young adults the first remedy for high non-HDL cholesterol would be exercise and losing extra weight, followed by eating a healthier diet, said Blankenberg.
Colin Baigent, director of the MRC Population Health Research Unit, at the University of Oxford, is quoted in the report as saying: “This is an important paper because it shows what could be achieved if, starting early in their 40s, healthy people were to start taking a statin so that their bad cholesterol is halved for the rest of their lives.
“Of course, despite the fact that statins are safe and well tolerated, many healthy people would be reluctant to take a statin from early middle age. But the striking findings of this study show that a policy of recommending such treatment might be a long-term investment that leads to a substantial improvement in the health of older people in the years to come.”
Abstract
Background: The relevance of blood lipid concentrations to long-term incidence of cardiovascular disease and the relevance of lipid-lowering therapy for cardiovascular disease outcomes is unclear. We investigated the cardiovascular disease risk associated with the full spectrum of bloodstream non-HDL cholesterol concentrations. We also created an easy-to-use tool to estimate the long-term probabilities for a cardiovascular disease event associated with non-HDL cholesterol and modelled its risk reduction by lipid-lowering treatment.
Methods: In this risk-evaluation and risk-modelling study, we used Multinational Cardiovascular Risk Consortium data from 19 countries across Europe, Australia, and North America. Individuals without prevalent cardiovascular disease at baseline and with robust available data on cardiovascular disease outcomes were included. The primary composite endpoint of atherosclerotic cardiovascular disease was defined as the occurrence of the coronary heart disease event or ischaemic stroke. Sex-specific multivariable analyses were computed using non-HDL cholesterol categories according to the European guideline thresholds, adjusted for age, sex, cohort, and classical modifiable cardiovascular risk factors. In a derivation and validation design, we created a tool to estimate the probabilities of a cardiovascular disease event by the age of 75 years, dependent on age, sex, and risk factors, and the associated modelled risk reduction, assuming a 50% reduction of non-HDL cholesterol.
Findings: Of the 524 444 individuals in the 44 cohorts in the Consortium database, we identified 398 846 individuals belonging to 38 cohorts (184 055 [48·7%] women; median age 51·0 years [IQR 40·7–59·7]). 199 415 individuals were included in the derivation cohort (91 786 [48·4%] women) and 199 431 (92 269 [49·1%] women) in the validation cohort. During a maximum follow-up of 43·6 years (median 13·5 years, IQR 7·0–20·1), 54 542 cardiovascular endpoints occurred. Incidence curve analyses showed progressively higher 30-year cardiovascular disease event-rates for increasing non-HDL cholesterol categories (from 7·7% for non-HDL cholesterol <2·6 mmol/L to 33·7% for ≥5·7 mmol/L in women and from 12·8% to 43·6% in men; p<0·0001). Multivariable adjusted Cox models with non-HDL cholesterol lower than 2·6 mmol/L as reference showed an increase in the association between non-HDL cholesterol concentration and cardiovascular disease for both sexes (from hazard ratio 1·1, 95% CI 1·0–1·3 for non-HDL cholesterol 2·6 to <3·7 mmol/L to 1·9, 1·6–2·2 for ≥5·7 mmol/L in women and from 1·1, 1·0–1·3 to 2·3, 2·0–2·5 in men). The derived tool allowed the estimation of cardiovascular disease event probabilities specific for non-HDL cholesterol with high comparability between the derivation and validation cohorts as reflected by smooth calibration curves analyses and a root mean square error lower than 1% for the estimated probabilities of cardiovascular disease. A 50% reduction of non-HDL cholesterol concentrations was associated with reduced risk of a cardiovascular disease event by the age of 75 years, and this risk reduction was greater the earlier cholesterol concentrations were reduced.
Interpretation: Non-HDL cholesterol concentrations in blood are strongly associated with long-term risk of atherosclerotic cardiovascular disease. We provide a simple tool for individual long-term risk assessment and the potential benefit of early lipid-lowering intervention. These data could be useful for physician–patient communication about primary prevention strategies.
Authors
Fabian J Brunner, Christoph Waldeyer, Francisco Ojeda, Veikko Salomaa, Frank Kee, Susana Sans, Barbara Thorand, Simona Giampaoli, Paolo Brambilla, Hugh Tunstall-Pedoe, Marie Moitry, Licia Iacoviello, Giovanni Veronesi, Guido Grassi, Ellisiv B Mathiesen, Stefan Söderberg, Allan Linneberg, Hermann Brenner, Philippe Amouyel, Jean Ferrières, Abdonas Tamosiunas, Yuriy P Nikitin, Wojciech Drygas, Olle Melander, Karl-Heinz Jöckel, David M Leistner, Jonathan E Shaw, Demosthenes B Panagiotakos, Leon A Simons, Maryam Kavousi, Ramachandran S Vasan, Robin PF Dullaart, S Goya Wannamethee, Ulf Risérus, Steven Shea, James A de Lemos, Torbjørn Omland, Kari Kuulasmaa, Ulf Landmesser, Stefan Blankenberg, Multinational Cardiovascular Risk Consortium
[link url="https://www.theguardian.com/uk-news/2019/dec/03/bad-cholesterol-levels-should-be-checked-from-age-of-25-study"]The Guardian report[/link]
[link url="https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(19)32519-X/fulltext"]The Lancet abstract[/link]