A likely reason for Africa’s low incidence of COVID-19 is lack of testing and surveillance. Research at the Zambia University Teaching Hospital morgue found that up to June 2021 SARS-CoV-2 was detected in around 25% of deaths – and in June the rate rose to 87% of all deaths – writes Christopher J Gill of Boston University in The Conversation.
This article updates research published in the British Medical Journal on 17 February 2021, and shows a subsequent significant increase in proportions of deaths involving COVID-19. See the link to the BMJ article information below.
Understanding the epidemiology of infectious diseases often rests heavily on the local resources available to conduct surveillance work. It is very easy to fall into the trap of believing that the absence of information about a given country or region means that diseases are not having an impact in those places.
The apparently low rates of COVID-19 on the African continent are an example of this.
Much of what we think we know about the impact of COVID-19 globally rests on aggregated data presented through portals like the Johns Hopkins COVID-19 website. Based on this, one could easily conclude that the pandemic hit the United States harder than anywhere else in the world and that Africa has largely been spared.
But COVID-19 spreads wherever the concentration of people allows. What distinguishes the US from most African countries is that the US has the most resources for disease surveillance in the world, including the US Centers for Disease Control and Prevention.
The existence and reliability of data may differ as a function of local capacity, expertise, resources and political will. In Africa, the highest concentration of cases appears to be in South Africa – a relatively high-income country with excellent capacity and resources for testing and surveillance.
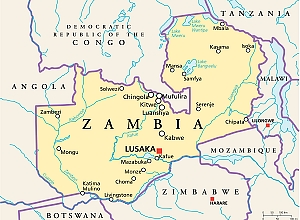
We have been measuring the fatal impact of COVID-19 in Zambia’s capital Lusaka. It has shown us how difficult it is to do systematic surveillance. And yet the global health community has largely treated the low rates in most of Africa as a mystery. The most likely explanation is that the necessary resources for surveillance are inadequate and hence that we are not seeing a complete picture about what is really going on.
For more than four years, we have been collecting data on infant deaths as part of a project to study other diseases. When the COVID-19 pandemic broke out, we were able to amend our surveillance work to include this new virus and to determine what proportion of individuals across all ages in Lusaka tested positive through postmortem sampling.
This was work funded by the Gates Foundation, and we shared our findings with the Zambian Ministry of Health.
These data are representative and generalisable because we are sampling at the University Teaching Hospital morgue, which captures nearly all deaths that occur in the city across all age groups. While we lacked the resources to sample all deaths – 30 to 40 deaths per day is quite typical – we sampled a random sub-set of those.
What we observed from June to September 2020 was that roughly one in five deceased individuals tested positive for SARS-CoV-2 in our molecular laboratory in Lusaka. The rates we were seeing were roughly 10 times higher than what was being reported officially at the time.
Since that initial report, we have continued to monitor COVID-19 deaths at the same morgue. The situation has clearly grown worse. Up to June 2021, we were detecting SARS-CoV-2 in roughly 25% of deaths. But in June itself the rate rose to an astonishing 87% of all deaths.
We are currently in the process of an excess mortality analysis, comparing the COVID-19 year against the background rate of seasonal mortality over the preceding three years. This will help us better measure the impact of COVID-19.
A lack of surveillance
Our team is based at the University Teaching Hospital morgue. We attempt to enrol every third to fifth death that comes through, approaching the family or next of kin to obtain informed consent. Our consent rates have been very high (about 90%).
We then obtain some clinical information about the events leading to the fatal illness, and obtain a nasal swab sample for testing. We use the US Centers for Disease Control’s testing kits, which are considered to be a global gold standard.
If we included detection of SARS-CoV-2 at any level of signal intensity on the PCR assay, we found it in 19% of all deaths between June and September 2020. Nearly three quarters of those deaths occurred outside medical care. Of these, none had been tested for the virus prior to death. Among the deaths that occurred at a hospital, only about a third had been tested prior to death.
This tells us that the seemingly low rate of COVID-19 reported elsewhere was explained by a lack of systematic surveillance. COVID-19 seemed rare only because testing was rarely done. Of the 70 COVID-19 deaths we detected out of 342 deceased individuals, only six had been tested for COVID-19 before they died. And yet nearly all had had symptoms suggestive of COVID-19 – cough, fever, shortness of breath.
In Zambia there are insufficient funds and capacity to do thorough surveillance. Zambia ranked 117th out of 128 countries in terms of economic competitiveness back in 2007.
Wider picture
The key concern is whether these results are unique to Zambia. We doubt it. It seems most likely that COVID-19 is having a severe impact in many (possibly most) parts of Africa, but this is simply going undocumented.
As we have seen in the US – which has largely reopened its society after vaccinating over 180 million citizens – the only way out of this human calamity is vaccines.
Only a few percent of Zambia’s population has received any COVID vaccine. And while the goal is to vaccinate the population, Zambia’s access to vaccines is severely limited. We hope that the COVAX initiative may change this situation.
As long as Africa’s “low COVID-19 rate” continues to be viewed as a puzzling enigma rather than a sign of inadequate surveillance, African countries will be at the back of the bus to get these life-saving commodities. In all likelihood, this is a catastrophe that is occurring on a continental scale yet is simply going unreported and hence unappreciated.
To solve a problem like COVID-19, it is obviously essential to have accurate information about the true status of the situation.
* Christopher J Gill is an Associate Professor in the Department of Global Health, and an Infectious Diseases Specialist, at Boston University in the United States.
* This article is republished from The Conversation under a Creative Commons license. The link to the original article is below.
COVID-19's impact in Africa 'vastly underestimated’ — BMJ study
See also from the MedicalBrief archives
‘Most South Africans have had COVID-19' — National Blood Service study
Africa’s first COVID-19 vaccine technology transfer hub
Africa's COVID-19 case fatality rate now higher than global rate
Unravelling why African ICUs have the world's highest COVID-19 mortality rates