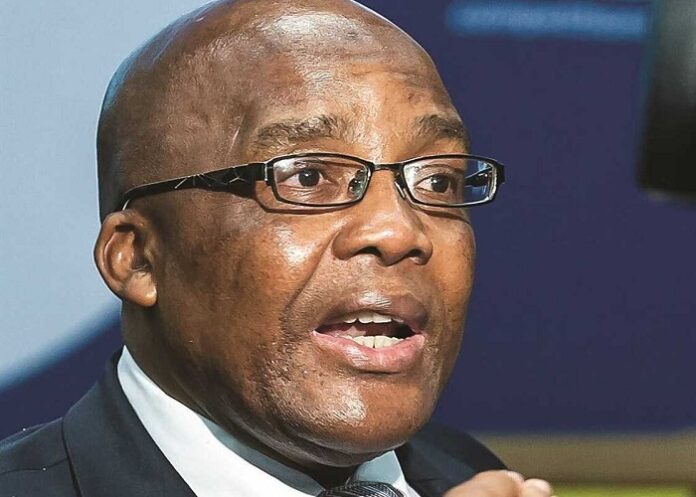
Since Dr Aaron Motsoaledi’s first appointment as Health Minister 15 years ago, South Africa’s HIV treatment programme has grown to be the world’s largest, and his push for access to new tuberculosis drugs has been lauded.
But he’s also been criticised for failing to implement long-lasting health system solutions and for controversial comments on the reason for collapsing health services.
Now, he is focused on accelerating the implementation of the NHI, and in a Zoom interview, Bhekisisa writer Sean Christie gets an insight into the man and his mission.
He writes:
After pleasantries, I explain to the Minister that I am hoping for a form of life story share.
Motsoaledi responds with a swift biographical flyover, with bullet points.
He says he was born, raised and mostly educated in Sekhukhuneland, which straddles the border of present-day Limpopo and Mpumalanga Provinces.
After some false starts he studied medicine at the then University of Natal (today the University of KwaZulu-Natal Nelson R Mandela school of medicine), doing his internship at King Edward VIII Hospital. After graduating, he worked for a year at Masana Hospital (now Mapulaneng) in Bushbuckridge, and in 1986 opened a private surgery in Sekhukhuneland, in a town which grew up around a hospital: Jane Furse Memorial.
Here he remained, working as a community GP until the advent of democracy, when he became a member of the provincial legislature in Limpopo.
“I would later serve as MEC for Education, Transport and Agriculture. In 2009, I was sent to Parliament, and appointed Minister of Health (until 2019). I have served in Cabinet ever since, and started my second term as Health Minister in June. Thank you,” he concludes, the way an emergency responder might say, “over”.
All of this information is already recorded in many an online bio. Included in such write-ups is ample recognition of his (more or less undisputed) contributions in the healthcare sector, including a massive expansion of HIV, TB and maternal health services. They also make reference to several controversies, including Motsoaledi’s scapegoating of foreigners as the cause of collapsing health services and overcrowded hospitals, and that he was Minister when the Life Esidimeni tragedy took place.
But I am more interested in what is absent from those writings: the experiences behind the bullet points, both good and bad.
Happily, when asked, Motsoaledi was only too willing to depart from his fact-sheet approach.
Barefoot in Phokwane
“I used to go to school without any shoes, like all rural kids then. In fact, I got my first pair of shoes and first pair of long trousers only after passing primary school,” he says. His bare feet saw the inside of many primary schools, because his school principal father was moved around a lot.
“I was one of nine siblings. Our home was the village of Phokwane, but I moved with my father (Kgokolo Michael Motsoaledi) whenever he was posted to a new village school.”
A standout student, who passed standard 3 (grade 5 today) “with absolutely flying colours”, Motsoaledi was allowed to vault standard four. He excelled at sports, always taking the baton last in the relay race.
He stopped playing team sports a long time ago. “For years, my thing was walking – I used to walk the streets, 20km at a time up to three times a week – but my security detail put a stop to this when I became a Minister.”
Political awareness
After primary school, he attended Setotolwane High, 20km outside Polokwane, a boarding school whose alumni include Mamphela Ramphele.
“Although we were a rural school there was a keen awareness of the struggle to end Bantu education. Ninety percent of our teachers were Afrikaners, for one thing,” says Motsoaledi, who joined fellow students in disrupting school activities on 16 June 1976, after word reached them of the Soweto youth uprising.
“On that day some of us slept in a tree, because our school library burned down, and we were all regarded as culprits by a certain Colonel Van Zyl, who had arrived to attack us.”
He made it through matric without further mishap, scoring marks that secured him a place in the University of Natal’s medical school.
Unable to afford the fees, Motsoaledi taught for a year, but by the time he was ready to enrol again the university had been told it could no longer accept black students.
“The government had decided to separate the races into their own separate ethnic universities. I was told I would have to attend the recently opened Medunsa (the Medical University of South Africa, today Sefako Makgatho Health Sciences University)in Garankuwa.”
He completed a pre-medical course at the University of the North, at Turfloop (now University of Limpopo), and by the time he finished this, the University of Natal was again accepting black medical students, “after a big protest against the removal of Africans”.
Link between struggle for medicine and liberation
“I was really highly politicised by the time I arrived in Durban, an angry young black person,” says Motsoaledi, who found “the mood of organising” on campus different from what he had experienced in Limpopo, “where the level of political activity was exceeded by the level of repression”.
In his first week, a group of activists arrived from Johannesburg to launch the Release Mandela campaign on campus. Motsoaledi was intrigued to learn that one of the speakers was the medical school dean, Theodore Sarkin.
“I was not used to that, because at the university I had come from we viewed the white university authorities as enemies. Ever since high school that’s how I had viewed every white person, in fact,” says Motsoaledi, who had a personal stake in the campaign because his uncle, Elias Motsoaledi, was at the time imprisoned alongside Mandela on Robben Island.
Sarkin, he says, narrated a simple and compelling story.
“He said something to the effect of, look, I’m a professor in medicine working at King Edward VIII Hospital, which is always overcrowded, and there are days when I have to kneel down to examine a patient because he’s lying on the floor, or sleeping under the bed, because there’s no space. Meanwhile, there’s a big hospital down the road with lots of empty beds in it – Addington – but I cannot take our excess people there because it’s a whites-only hospital. I’m a professor of medicine, yet I can’t help my patients.
“He said he believed that Nelson Mandela held the only key to this problem.. he wanted him out of prison so we could start a new country together.”
Motsoaledi thereafter embraced the province’s brand of politics, which emphasised non-racialism. He joined the student representative council in his second year, and would later become its president, working alongside Sarkin.
“He really helped us a lot. Whenever security police came on to campus, they reported to him first and he would delay them so that we could hide, or dispose of incriminating materials,” Motsoaledi recalls.
“Now,” he says, “I’m emphasising this episode because it made me realise there’s a link between the struggle for medicine and the struggle for liberation, and I did not need to think of my studies and my political activities as separate arenas.”
A GP underground – with a briefcase full of cash
Motsoaledi would become the first correspondent secretary of the Azanian Students Organisation, (later the South African Students Congress), and towards the end of his time in Durban he was working underground, “helping comrades on the run to cross a border into exile”.
After graduating and moving back up north, he thought it was all over, but there came a day in 1987 when a man walked into his surgery in Jane Furse, and announced that he was a member of the ANC’s then banned military wing, uMkhonto weSizwe, living underground.
“He said he had lost contact with his handlers outside the country, and that his orders in the event of this happening were to report to me. I said, ‘How do you know I am not a police spy?’ and he said, ‘Well, if that’s the case, the leadership has misled me’.”
Motsoaledi was gobsmacked, but decided to get involved with the local cell, financing his new comrades’ operations from his own pocket, and helping with logistics.
Years later, his contact handed him a letter addressed to Chris Hani, chief of staff of uMkhonto weSizwe.
“He asked me to hand the letter to Hani. I thought this was very ambitious and mad — I could not believe Hani knew of this particular man and our cell, but he insisted and so I visited my uncle, Elias Motsoaledi, who was then living in Mzimhlophe in Soweto, and he handed me over to Tokyo Sexwale, who took me to this house deep in Zola, where I found Chris Hani sitting in a bedroom,” says Motsoaledi, adding that he was “shivering with nerves”.
“I was completely starstruck, but he was such a simple, humble person. After reading the letter he promised he would contact me at a later date, and that he was happy I was helping these fellows.”
Motsoaledi met Hani again at a hotel in Thohoyandou in the company of Tokyo Sexwale.
“Inside the hotel room he gave me the proverbial briefcase filled with cash, and said, ‘go and help those fellows but also help yourself, because you have been using your own resources’, and I assured him I would not do that, and that I regarded it as a contribution to the struggle,” says Motsoaledi.
His involvement in the underground grew until his commander was killed in a house raid by government security forces, destroying the cell.
Motsoaledi would continue his political activism until 1994, when he joined the provincial legislature in Limpopo.
Uncle Elias: ‘We lived together in my mother’s house’
He has mentioned his famous uncle Elias a few times, but always obliquely.
“How well did you actually know him?” I venture.
“Well, look,” he says, beginning his answer the same way he began all previous answers, “his involvement in the Rivonia Trial and his subsequent imprisonment on Robben Island all happened before I went to school, and for years afterwards his name was hardly ever mentioned because in rural areas then, if you spoke about political leaders it was in corners, in whispers.”
He only came to fully appreciate his uncle’s contribution to the struggle when he attended university, and as soon as he could afford it, Motsoaledi travelled to Cape Town and visited him on Robben Island.
After Elias Motsoaledi’s release in 1989, the two men became close.
“He came to Sekhukhuneland on Walter Sisulu’s instructions, who told him to mobilise the traditional leaders. We lived in my mother’s house. I was moving around with him, organising with him,” he recalls.
Elias Motsoaledi died on the day Mandela was inaugurated as president of South Africa, a month after his nephew was elected to represent the ANC in the newly established Limpopo provincial legislature.
“I like to think he departed believing his sacrifice was not in vain,” says Motsoaledi.
I ask about his own decades-long contribution to the liberation struggle, especially as it pertains to healthcare.
“Look, as students we really believed we could form an alternative health system in this country,” he says.
“Thanks to people like Sarkin, we were aware of the Alma-Ata Declaration of 1978, which insisted that health is a fundamental human right, and that expanding primary healthcare was the solution to achieving health for all by the year 2000.
“We had also read the report called Apartheid and Health, which came from the 1981 meeting of the World Health Organisation Africa region. It described apartheid as the very negation of health for all, something that has to be totally eradicated before that vision could be realised.
“So we had this idea that you had to first be a soldier to fight for liberation, then healthcare delivery would follow. Of course, this isn’t what happened.”
In his reckoning, the dream of health for all was thwarted at the dawn of democracy, “when private healthcare and medical schemes accelerated, starting a new and more brutal form of apartheid, dividing people in terms of what one has in resources to pay for healthcare services”.
He illustrates his point with a reference to the so-called ABCs of cardiopulmonary resuscitation.
“After something like a motor vehicle accident, when a victim is unresponsive, we were taught as medical students to check the airways, breathing and circulation, and then you can administer drugs as necessary.
“Now when you find someone like that on the road, the first thing that must be checked is whether they have medical aid or not. When triage is being done at the scene, it’s no longer about how sick you are; it’s about whether you have medical aid, in which case you will get a different quality of care.
“I find that completely unacceptable.
“Financial apartheid is trickier to fight than racial apartheid, because back then you could see your enemy; now there’s an integration of people who were formerly enemies, including the cream of the black nation.
“I’m talking about public servants, doctors, nurses, teachers, police, the army, members of parliament, even the judiciary – they have all been bundled together, and are getting very heavy subsidies from the fiscus to be on medical aid, whereas those who are not employed, or in lower jobs, have been left to fend for themselves, alone.”
NHI: Why getting it done is personal
I can sense the elephant in the room – National Health Insurance (NHI) – shifting its feet in the corner. Although this controversial NHI Act has a history going back to 1994 and the coming to power of the ANC, it is Motsoaledi who is seen as NHI’s midwife, and who who oversaw the development of the policy discussion documents that preceded the signing into law of NHI in May.
He also presided over the implementation of a series of expensive and less-than-encouraging NHI pilot projects in various parts of the country.
What he says next reinforces the view that for him, getting NHI done is a personal mission, driven (perhaps at the cost of expediency?) by long-cherished revolutionary ideals.
“The way NHI is being very vehemently opposed – I may even say verbally violently so – tells you we have never had a revolution in healthcare.
“There was a clear revolution fought to bring forth equal education for all. The 1976 youth uprising saw to that, and much later, Fees Must Fall provided a reminder that if you mess around in that sector, there will be an uprising.
“There has been nothing like that in healthcare.”
Beneath the obvious outrage there seems to be a note of fatigue, or resignation. It is one thing to dream, another to deliver the dream in a real-world context, especially one featuring an increasing number of steep barriers, ranging from the poor state of the economy to the fact that Motsoaledi’s party, the ANC, lost hegemony in the general elections, and now leads the country as the primary partner in a government of national unity comprising 11 parties, only four of which support NHI outright.
Our time is up, and the Minister signs off with the same formal politeness with which he began the conversation. He is gone before I can mention that we had, in fact, met before, at the 2018 TB Conference in Durban.
It is a story worth sharing, I think.
I was working for a medical non-profit group, and for several years we had been pushing hard for better treatment options for patients with drug-resistant forms of TB.
The National Department of Health (NDoH) had secured limited access to newer drugs through special agreements with pharmaceutical companies but could not allow blanket access because the drugs were still undergoing clinical trials, and the WHO had not yet recommended their routine use.
By 2018, however, the department’s own evidence showed the new drugs were safer and more effective than the old ones. At the meeting with Motsoaledi and his TB team, we suggested that if the country were to announce it could not wait any longer to offer the new drugs to all patients who needed them – that to do so would frankly be unethical – it would push the WHO to hurry up and recommend their use.
Motsoaledi turned to the head of his TB directorate, Norbert Ndjeka, and said: “I think we must do it.”
A public announcement followed the next day, and not long afterwards the WHO recommended these same drugs be made routinely available.
A classic act of activism, led by a man who remains, at heart, a fighter.
See more from MedicalBrief archives:
Motsoaledi to increase push for NHI
Motsoaledi era: HIV/Aids success but public healthcare failures
Motsoaledi lashed for saying illegals are burdening health system
Motsoaledi wins prizes for his efforts in fighting TB