Almost half of South Africa’s nurses due to retire in the next 15 years and with only universities accredited to offer the professional nurse programme there will be an almost 80% drop in new nurses in three years’ time, reports Spotlight.
The national spokesperson of the Democratic Nursing Organisation of South Africa (DENOSA), Sibongiseni Delihlazo, says, “This is a ticking time-bomb that is just waiting to blow up in the face of South Africans.”
According to 2020 statistics from the SA Nursing Council (SANC), the current age demographics of registered nurses and midwives are heavily skewed towards older practitioners, with fewer than a third under 40. The statistics show 27% of registered nurses are in their 50s, 26% in their 40s, and only 21% in their 30s (see table).
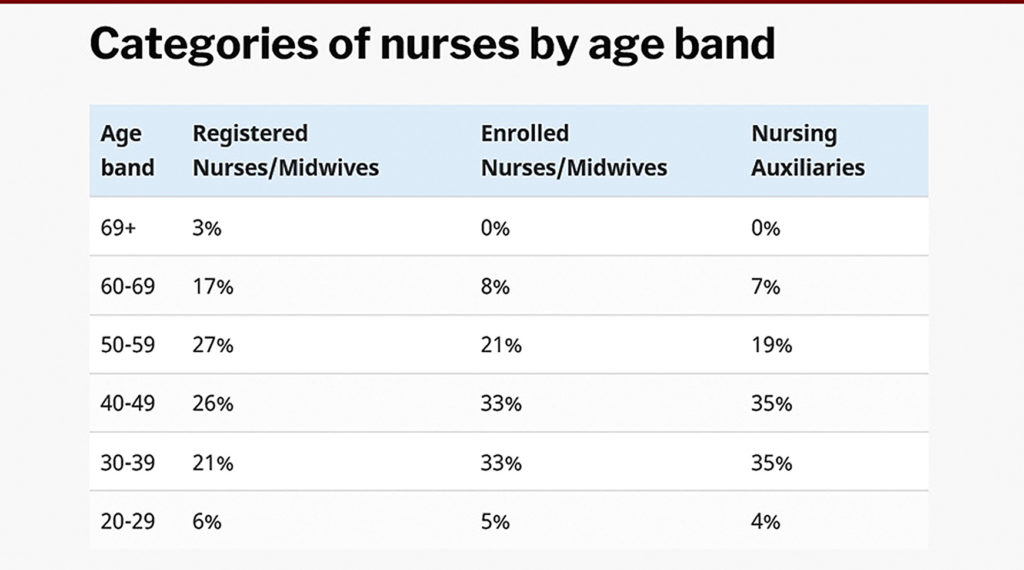
The demographics of enrolled nurses and nursing auxiliaries are only slightly more evenly distributed.
The set retirement age for nurses in the public sector is 65, although some extensions are allowed. This means, in short, that in 15 years, 47% of registered nurses will have retired. The same applies to about 26 to 30% of the enrolled nurses and nursing auxiliaries.
‘We have a crisis’
“We have a crisis of an ageing workforce,” says Prof Laetitia Rispel, the South African Research Chair on the Health Workforce at Wits University. She said while this was an international problem, South Africa’s relatively young population made is worrying.
“It’s not just the replacement of the actual individuals, but you also have to look at the cumulative experience and wisdom in the health system and that’s not going to be replaced unless we sort of take action now,” she said.
The Rural Health Advocacy Project (RHAP) has done various consultations with stakeholders in the nursing field in the past months. Project officer in its human resources for health programme, Lungile Gamede, said while there were no exact data available on how this compares across the nation, “We have no doubt that communities living in rural areas will bear the brunt of the severe shortages, which will be exacerbated when almost half of the registered nurses and midwives retire round about the same time.”
According to South Africa’s 2030 Human Resources for Health Strategy, if nothing substantial is done it is projected that by 2025, there is likely to be a shortage of about 34 000 registered nurses in primary health care.
Historical causes
The current and anticipated future shortages seem to come down to overall systemic issues as well as particular shifts in nursing. “It’s an underinvestment in human resources for health in general and a historical neglect of nurses and nursing,” said Rispel.
Professor Helen Schneider from the School of Public Health at the University of the Western Cape said there has been an “increasing professionalisation of nursing with longer, more expensive training, with growth of expectations in status and remuneration”. She said this has created issues of supply and affordability, and growing divisions of labour at the base of the system.
Funding of staff contributes strongly, according to Delihlazo. “Poor HR planning as well as continuous reduction of budget for funding nursing education by government are at the core of the problem.”
President of the Young Nurses Indaba (YNITU), Lerato Mthunzi, said working conditions added to the problem, making the nursing profession less attractive.
She said because of burnout and the “brain drain”, many have left the profession or the country for better working conditions, putting pressure on those who remain. General wards now have ratios of about one nurse and assistant to 20 or 30 patients, she said, compared with the norm of around five to one, shifting the focus from quality care to just managing.
Gamede said this crisis would have a negative effect on the ability to provide primary health care, given the important role nurses play in this, as well as undermine the health system’s ability to focus on TB and HIV care. Key health indicators, especially of children, and the general ability to reach the health-related Sustainable Development Goals (SDGs), would be compromised.
Issues with training
According to statistics published on the SANC website, the total number of nurses on its register has increased from around 238 000 in 2011 to around 280 000 in 2020. This amounts to an increase of 18%, roughly in proportion with population growth over the same period.
These numbers seem to indicate that South Africa has made little or no progress over the past decade in addressing its nursing shortages. Furthermore, recent setbacks in nurse training may mean that shortages will get worse before they get better.
In 2020, legislation changed to require all nursing education institutions (NEIs) to register as higher education institutions (HEI), which was previously only linked by university nursing departments. The CEO of the Nursing Education Association, Dr Nelouise Geyer, said: “This should improve the critical-analytical skills of graduates but the transition has created a significant gap in the number of graduates.”
Many smaller private schools had closed down, she added, because they could not afford to register as an HEI. Public nursing colleges did not meet the requirements, although the minister of Higher Education had created a transitional arrangement to let them qualify temporarily.
“The most challenging change is that only universities have been accredited to offer the professional nurse programme,” she told Spotlight. “This will result in an almost 80% drop in the production of professional nurses in three years’ time.”
Geyer is particularly concerned about the shortage of specialist nurses, as none had been trained during 2020 and 2021, she said, due to none of the specialist programmes having been newly accredited. She is not hopeful that many will resume next year.
The national Department of Health confirms that there are currently 17 universities accredited, 10 public, and 10 private nursing colleges. The total number of students who can be admitted for training per year per programme is around 5 900.
Mthunzi said she’d heard that those taking the new accredited courses were having a lot of problems with them. The lecturers also feel unsupported and frustrated, she added, often lacking the right qualifications. “This leaves them really behind in terms of being more effective or enabled to deliver content as required.”
Changing course
A response from the health department on these issues indicated that its focus is on “developing nursing education and practice nationally to cope with the demands and ensure alignment to nursing workforce planning”.
Mitigating the growing shortage of nurses would clearly start with tackling the challenges in the training sector as quickly as possible. Schneider said the new curriculum needed to be correctly implemented urgently, while Delihlazo said we should “reopen the previously closed nursing colleges as of yesterday” and increase training infrastructure.
Gamede said change could come by urgently accrediting more training institutions through strengthening the Community Services Programme, improving poor working and living conditions, and adjusting remuneration. To help equip nurses better, training should be more accessible and less centralised, with nursing education institutions being held more accountable.
Beyond the tricky business of training more nurses, effective steps towards realising the Human Resources of Health Strategy are crucial. On paper it looks strong and includes a focus on digital health technology, “the harmonisation of accreditation, registration, and regulation of NEIs”, and to “institutionalise functional governance structures with empowered, competent, accountable, and capacitated nurse/midwife leaders and managers at national, provincial, and district levels”.
Rispel, who was involved in the strategy-writing process, said that unfortunately, little had been implemented, but the starting point would be understanding what resources there are and need to be, and working towards this.
“One of the key recommendations made was the need for a highly specialised human resource intelligence and information system that should be set up in the national Department of Health, and that would be capable of developing credible planning models, abd able to collect information that we would be able to forecast and also highlight what policy levers should be utilised,” she said.
While various models have already been outlined in the strategy, it is clear that change would start with implementation.
“In our strategy, we certainly highlighted that regardless of which modelling was used, we will require an additional number of health workers,” Rispel said.
While the SANC did respond to media requests from Spotlight, it mostly shared statistics and did not provide substantive comment on other issues.
Spotlight article – Ageing nurses: A crisis on the horizon (Creative Commons Licence)
See more from MedicalBrief archives:
Private sector asks SANC to be allowed to train more nurses
Changed qualification requirements will exacerbate nursing shortage
SANC and National Education must together resolve nursing crisis — Solidarity
Scramble to fund nursing and medical intern posts
Crowdfunding supports medical students amid a nationwide doctor shortage
