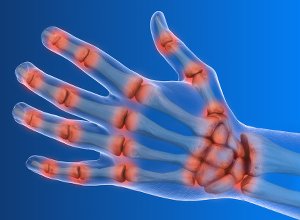
 Electro-stimulation of one of the nerves connecting the brain to the body, the vagus nerve, could provide a novel treatment approach for patients with rheumatoid arthritis, according to a pilot study presented at the Annual European Congress of Rheumatology (EULAR2019).
Electro-stimulation of one of the nerves connecting the brain to the body, the vagus nerve, could provide a novel treatment approach for patients with rheumatoid arthritis, according to a pilot study presented at the Annual European Congress of Rheumatology (EULAR2019).
"This is a really exciting development. For many patients suffering from rheumatoid arthritis, current treatments don't work, or aren't tolerated," said Professor Thomas Dörner, chair of the scientific programme committee, EULAR. "These results open the door to a novel approach to treating not only rheumatoid arthritis, but other chronic inflammatory diseases. This is certainly an area for further study."
The vagus nerve is the longest and the most complex of the 12 pairs of cranial nerves that originate from the brain. The name 'vagus' comes from the latin word for 'wandering'. This is because the vagus nerve wanders from the brain into the organs of the neck, chest and abdomen.
Recent advances in neuroscience and immunology have mapped circuits in the brain that regulate immune responses. In one of the circuits, the 'inflammatory reflex', signals are transmitted in the vagus nerve that inhibit the production of cytokines including tumour necrosis factor (TNF), an inflammatory molecule that is a major therapeutic target in rheumatoid arthritis. It is thought that, by stimulating the activity of this inflammatory reflex, innate immune responses can be modulated without abolishing them or producing significant immunosuppression.
In this pilot study, a novel miniaturised neurostimulator called a MicroRegulator was implanted into 14 patients with rheumatoid arthritis who had failed on at least two biologics or targeted oral therapies with different mechanisms of action. Patients were randomised to three groups who were either placebo, stimulated once daily, or stimulated four times a day for 12 weeks. At the end of the study, the patients who received once-daily stimulation were shown to have a better response than those on four-times-daily stimulation with two thirds meeting the EULAR good or moderate response criteria and a mean change in DAS28-CRP of -1.24. The mean change in DAS28-CRP* in the placebo group was 0.16.1
Cytokines (a broad and loose category of small proteins that are important in cell signalling) were also measured in the study with the actively stimulated groups showing a decrease of more than 30% in levels of Interleukin (IL) 1β, IL-6, and TNF-α. Implantation and stimulation were generally well tolerated with no device or treatment-related SAEs and two surgery-related adverse events that resolved without clinically significant effects.
"Our pilot study suggests this novel MicroRegulator device is well tolerated and reduces signs and symptoms of rheumatoid arthritis," said Dr Mark Genovese, James W Raitt endowed professor of medicine, Stanford University. "These data support the study of this device in a larger placebo-controlled study as a novel treatment approach for rheumatoid arthritis and possibly other chronic inflammatory diseases."
This study follows a proof-of-concept study which used reprogrammed epilepsy stimulators on the vagus nerve to demonstrate reduced systemic inflammation and improved disease activity in 17 patients with rheumatoid arthritis.
The study included 14 patients with active rheumatoid arthritis who had had an insufficient response to more than two biological disease modifying anti-rheumatic drugs (bDMARDs) or JAK inhibitors with more than two modes of action. All patients remained on stable background of methotrexate. The first three patients were implanted and stimulated after three weeks, following safety review board approval, the remaining 11 patients were implanted and randomised to one minute of stimulation once-daily, one minute of stimulation four times daily, or one minute of placebo stimulation.1
Abstract
Background: The inflammatory reflex plays a role in regulating innate and adaptive immunity through cellular and molecular pathways1. Activation of this neuroimmune reflex by electrical vagus nerve stimulation (VNS) reduced systemic inflammation and improved disease activity in a 17 subject rheumatoid arthritis (RA) proof-of-concept study using a reprogrammed epilepsy stimulator2. A novel miniaturized neurostimulator, the “MicroRegulator” (MR), was developed for a first-in-human pilot study in multi-drug refractory RA. Objectives: To assess the safety and efficacy of the MR in a double-blind study in active RA patients.
Methods: The MR was implanted in 14 patients with active RA and prior insufficient response to =2 bDMARDS or JAK inhibitors with =2 different modes of action; all patients remained on stable background of methotrexate. Three weeks after implantation, the first 3 subjects were stimulated 1 min QD and, following safety review board approval, the remaining 11 patients were implanted with the MR and randomized to 1 min of sham, QD, or QID stimulations for 12 weeks. Patients, rheumatologists, joint assessors and monitors were fully blinded to treatment arm. Subjects randomized to sham had their devices activated after the primary endpoint at 12 weeks. Clinical efficacy was measured by DAS28-CRP response and contrast-enhanced MRI (RAMRIS OMERACT). The pharmacodynamic response to VNS was assessed in blood using cytokine production in an ex-vivo bioassay (TruCulture).
Results: 14 patients were enrolled (mean prior bDMARDs= 4.8, mean DAS28- CRP= 5.94). Implantation and stimulation were generally well tolerated. There were no device or treatment-related SAEs and 2 surgery related adverse events (left vocal cord paralysis, Horner’s syndrome) that resolved without clinically significant sequelae. DAS28-CRP change at week 12 was (mean ± SEM): Open label QD= -1.44 ± 0.64, QD= -1.24 ± 0.88, QID= 0.38 ± 0.71, Sham=0.16 ± 0.21. Of QD stimulated patients, 4 of 6 had a EULAR good or moderate response. MRI measures of synovitis or osteitis did not change after 12 weeks of stimulation. RAMRIS erosion scores correlated with EULAR response (change ± SEM in erosion scores in EULAR responders = -2.2 ± 1.4 vs. 2.4 ± 0.96 in EULAR non-responders). The pharmacodynamic response to VNS was confirmed in actively stimulated groups with >30% decrease from baseline in bioassay levels of IL-1β, IL-6, and TNF-a at week 12.
Conclusion: The novel MR device and stimulation was well tolerated independent of the two surgery-related events. MR associated stimulation reduced signs and symptoms of RA in a meaningful number of highly drug-refractory subjects. No clinical improvement was observed in the sham group. These initial pilot data support the use of the MR in a larger blinded sham-controlled study in patients who have failed biologics or targeted oral therapies as a novel approach for treatment of RA and other chronic inflammatory diseases.
Authors
Mark C Genovese, Norman Gaylis, David Sikes, Alan Kivitz, Diane M Horowitz, Charles Peterfy, Yaakov Levine, David Chernoff
[link url="https://www.sciencedaily.com/releases/2019/06/190614082931.htm"]EULAR2019 material[/link]
[link url="https://ard.bmj.com/content/78/Suppl_2/264.1.share"]EULAR2019/BMJ abstract[/link]
