A common and popular food industry carbohydrate is being researched as a possible treatment for cancer and other diseases, including tuberculosis, writes Professor Admire Dube from the University of the Western Cape in The Conversation.
Curdlan, a name derived from the word “curdle”, is a popular carbohydrate, and is commonly used as a thickener and stabiliser in everything from sausages to milk substitutes.
More recently, it has caught the eye of the pharmaceutical industry. That’s because curdlan, itself produced by bacteria, is able to trigger an antibacterial response in a range of environments and organisms. Among other uses, researchers are looking at curdlan as a possible treatment for cancers and other diseases.
One of those is tuberculosis (TB), the infection responsible for killing more people than any other infectious disease in human history. South Africa has one of the world’s highest TB burdens – along with 29 other countries including India and China. These countries contribute 86% of the globe’s 10m annual TB cases. South Africa’s combined burden of TB, TB/HIV and multi-drug resistant TB (MDR-TB), driven by socioeconomic factors and its high HIV numbers, is especially worrying.
Existing remedies made up of cocktails of antibiotics are not effective against MDR-TB. This has sparked interest in finding alternative treatments. It’s why our research group at the School of Pharmacy at the University of the Western Cape, and others, are beginning to test the efficacy of curdlan as a potential drug candidate.
In a recent paper, for instance, we show very promising results for the potential treatment of TB using curdlan-based nanoparticles.
How TB infects
Our work centres on developing host-directed therapies using curdlan. Such treatments essentially let the human immune system do the heavy lifting. This is done by activating its natural antibacterial mechanisms while controlling the inflammation that results from such activation.
Inflammation is a signal that the immune system is working. But if inflammation is out of control it can cause major damage to human tissue, as seen in severe COVID-19 infections.
Research has already shown that host-directed therapies hold immense potential for the treatment of TB.
To understand how these therapies work, it’s important to understand how TB infection unfolds in the human body.
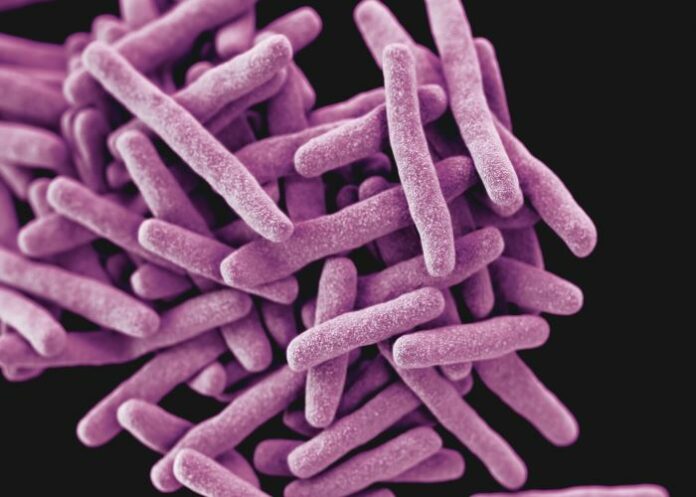
Primary TB infection occurs when a person inhales aerosol droplets, released by contagious individuals, that contain Mycobacterium tuberculosis (M.tb). This is the bacterium that causes TB. Once inhaled, M.tb quickly makes its way to the lung’s alveolar space, comprising tiny air sacs sitting at the end of the bronchioles.
Here it is absorbed by what’s known as alveolar macrophages, the lung cells that are usually the first line of defence against pollutants and pathogenic organisms. Typically these macrophages would trigger an immune response in the body. But M.tb has evolved so cannily that it eludes or switches off this immune-triggering response in the macrophages. These alveolar macrophages become its infection headquarters; the bacterium remains concealed within these cells.
For any treatment to be successful, it has to navigate a host of obstacles to reach M.tb. It must make its way through complex lung lesions, then penetrate the cell membrane of macrophages and other host cells, and finally be taken up by the M.tb sitting within these cells.
That’s where nanoparticles enter the picture.
Tiny ‘snipers’
Nanoparticles are extremely small. They range from between one to 100 nanometres; for some perspective, there are a million nanometres in a single millimetre. In theory, and as is being shown in laboratories and existing treatments for other conditions like cancer, nanotherapies allow drugs to target pathogens with sniper-like accuracy. They also have the potential to tackle patient non-compliance that can lead to drug resistant TB.
The reasons for non-compliance are varied and complex, but the duration of the therapy itself is a factor. Existing treatments require that, depending on the severity and progress of the disease, patients take many drugs over as many as six months. The course of treatment for MDR-TB lasts up to 24 months.
This high pill load, with sometimes toxic side effects, has been shown to overwhelm patients. Many do not return to clinics and hospitals for check-ups, especially when they feel better after a few weeks. Some stop taking their medication. This could be behind the rise of drug resistant strains. Such non-compliance is also believed to be the cause of South Africa’s comparatively high TB mortality.
Traditional drugs are taken orally or intravenously. They travel throughout the body via the blood circulatory system. Many drug molecules do not reach their targets, staying in the body where they cause several negative side effects.
That’s where nanoparticle-based treatments have the upper hand: they are extremely targeted and their release into the system is very controlled. Smaller doses are required and there is less dispersion around the body, meaning fewer side effects.
Promising findings
All of these factors suggest that nanoparticle-based treatments may be the right approach to take against TB. And two interesting findings from our study bolster the case.
One, we observed the production of what’s known as pro-inflammation cytokines, a signalling molecule that triggers an antibacterial effect in immune cells. This meant that the nanoparticles were doing what they were meant to do.
Second, we found that the M.tb bacteria in the immune cells were considerably reduced over a 72-hour period.
These results suggest that curdlan nanotherapeutics are an avenue worth exploring in treating TB. There is much more work to be done, but it’s an important step towards tackling TB – in South Africa and everywhere else.
Study details
Physicochemical and Biological Evaluation of Curdlan-Poly(Lactic-Co-Glycolic Acid) Nanoparticles as a Host-Directed Therapy Against Mycobacterium Tuberculosis
S D’Souza, S M Du Plessis, S Egieyeh, R B Bekale, R E Maphasa, A F Irabin, S L Sampson, A Dube.
Published in The Journal of Pharmaceutical Science on 14 September 2021
Abstract
Nanoparticles (NPs) that can activate macrophages infected with the tuberculosis causative pathogen Mycobacterium tuberculosis, could be an effective host directed therapy for the disease. In this study, curdlan was conjugated to poly(lactic-co-glycolic acid) (PLGA) to produce immunotherapeutic NPs. Various physicochemical characterisations were used to evaluate the curdlan-PLGA copolymer and the NPs. Molecular dynamics and simulation studies were used to characterise the interaction between curdlan, on the polymer and on NPs, with the Dectin-1 macrophage receptor. NPs with varying curdlan densities were evaluated for their effects on the production of pro- and anti-inflammatory cytokines in M. tuberculosis infected RAW264.7 macrophages. The killing efficacy of the NPs against intracellular M. tuberculosis was assessed. Physicochemical characterisation of the curdlan-PLGA copolymer and NPs indicated successful formation of curdlan-PLGA copolymer and NPs of varying curdlan density (0-8% w/w) had sizes between 330 and 453 nm. Modelling studies showed curdlan to have a strong affinity for Dectin-1. Cytotoxicity assays showed the NPs to be non-toxic over 72 h. The proinflammatory cytokine TNF-α was found to be significantly upregulated by the NPs. The NPs reduced intracellular M. tuberculosis burden over 72 h. These NPs are a promising host directed therapy for intracellular eradication of M. tuberculosis.
* Admire Dube is associate professor, Pharmaceutical Sciences, University of the Western Cape
See more from MedicalBrief archives:
NIH launches prevention trial of people exposed to multidrug-resistant TB
TB treatment outcomes good for multidrug-resistant TB/HIV co-infected patients who start ART
Shorter, simpler DR-TB regimen in the pipeline for South Africa