 Within a week, the 'revolutionary' HIV drug dolutegravir has gone from being highly regarded to being the subject of international warnings. Health-e News reports that recent data from a Botswana study linking it to birth defects has seen the World Health Organisation, European Medicines Agency and the US Food and Drug Administration, unanimously issuing warnings statements.
Within a week, the 'revolutionary' HIV drug dolutegravir has gone from being highly regarded to being the subject of international warnings. Health-e News reports that recent data from a Botswana study linking it to birth defects has seen the World Health Organisation, European Medicines Agency and the US Food and Drug Administration, unanimously issuing warnings statements.
Heralded as a breakthrough for the fight against HIV, and just as the country is embarking on a massive shift in its HIV treatment strategy based on this drug, the news has caused global panic. What does this mean for the biggest HIV treatment on earth, and for the women who make up the majority of its users? While some fear this news could destabilise South Africa’s remarkable progress in the fight against HIV, others caution against sounding the alarm bells too soon.
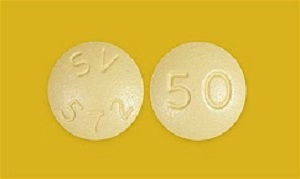
The report says dolutegravir is not just a new HIV drug, it has been described as a breakthrough weapon in the global fight against HIV. The low cost and comparatively mild side-effect profile have made it an attractive option for treatment programmes, especially in developing countries where savings on drugs can make it possible for significantly more people to be treated.
The possible link between neural birth defects which could impact the development of the brain and spine and dolutegravir was recently discovered in an ongoing observational study in Botswana, which switched its first-line HIV regimen to the drug in 2016. The study found four cases of neural tube defects in 426 women who have become pregnant while taking the drug.
While Professor Francois Venter from the Wits Reproductive Health and HIV Institute said this is not yet statistically significant, and could potentially be related to other factors, it prompted the EMA to issue a direct warning stating that: “Dolutegravir HIV medicines should not be prescribed to women seeking to become pregnant”.
The report says the WHO and FDA were more tempered in their guidance urging health care professionals to make women aware of these potential risks but not directing that it should stop being prescribed to women who might fall pregnant. They also noted that pregnant women on dolutegravir should not be switched hastily to different regimens as there is an increased risk of transmitting the virus to the baby.
But, despite the public concern globally, very little has been said about the impact of this news on the country most affected, not to mention being set to be responsible for a massive portion of the drug’s future market. South Africa has the largest HIV treatment programme in the world: 4.2m receiving antiretrovirals and, as promised by President Cyril Ramaphosa in his state of the nation address, this will be increased by 2m people by 2020.
The report says dolutegravir has been described as the main reason this goal is attainable. The National Department of Health had already planned to introduce a dolutegravir-based first line regimen to replace the existing regimen, hoping to switch the majority of patients starting from last month. But the introduction has been put on hold due to registration delays with the newly-formed South African Health Regulatory Products Authority which replaced the Medicines Control Council.
“It’s a massive curve ball,” said Venter. “It’s come at exactly the wrong time for South Africa and affects exactly the vulnerable group we are trying to protect: young women.”
Cost-savings threatened
According to a 2017 paper published in the South African Medical Journal, a dolutegravir-based regimen could translate into initial cost-savings of 20% of the country’s annual ARV budget. When volumes are met, when the majority of patients have been switched to the regimen, cost-savings could reach 50%. Venter said this is largely due to the price of the raw materials used to manufacture the drug. “The benefits of the drug are huge and it would be a tragedy if these results are confirmed and we lose it as a treatment option for many women,” he said.
HIV expert and technical advisor to the Department of Health, Dr Michelle Moorhouse said, to make matters worse, the drug has some other significant benefits for women. “It is a very tricky situation as dolutegravir is a great drug, and for those women who are using effective contraception, then it remains a great option,” she is quoted in the report as saying.
Many other existing HIV drugs interact with common forms of contraception, making treatment more difficult for many women. But as the health department has already made concrete plans to embark on a completely dolutegravir-based regimen, Dr Yogan Pillay, the deputy director general for HIV, said in the report that they are “following this very closely”. “Next week we will convene a meeting of experts to discuss our options based on the World Health Organisation guidelines,” he said.
He said the department is concerned about the financial impact of changing the dolutegravir guidelines, but that the first priority was the clinical well-being of patients adding that a possible option is to continue with the current regimen for women of reproductive age and offer the dolutegravir regimen to others.
But, said Venter, that this is problematic because women already make up about 70% of the total patients on HIV treatment in South Africa and it is ethically questionable to offer them a sub-standard option compared to men. “One thing I am angry about is that no-one funds drug studies on pregnant women,” he said. He said that “every now and again we get a signal from women that something is wrong” only after the drug has been approved and is in use instead conducting prior research which would identify “possible risks so we are able to prepare for that beforehand”.
“Governments, drug companies and funders haven’t invested in these studies and the argument is often that is unethical to test in pregnant women, but I argue the opposite. It’s unethical not to do this research.” He said the Botswana case is a “massive experiment on pregnant women without the safety and monitoring we have in normal clinical studies”.
Moorhouse, also from the Wits Reproductive Health and HIV Institute, cautioned against alarmist reactions to the warnings, the report said. “I have to say this is an early signal, which we need to take seriously, but we have seen similar signals before with other drugs, which over time turned out not to be the problem we anticipated,” she said.
There are a number of other studies underway which could clear up the link and potentially clear dolutegravir’s association with this serious potential side-effect – as well as clear the way for South Africa to more easily reach its treatment targets. “Until we better understand this signal from these ongoing studies, we have to exercise caution in using dolutegravir in women who are pregnant or desiring a pregnancy,” said Moorhouse.
“We simply need to introduce the necessary precautions as outlined in the various regulatory and other documents, while we wait for the clearer picture to emerge for the ongoing studies and data analyses,” she said. But she said the benefits of the drug, including the fact that it has shown no development of resistance in any patients, should not be overshadowed by this “signal”.
“I really do want to caution against panic,” she said. And while the idea of the drug as a panacea might be losing favour, she said in the report that “dolutegravir should not be heralded as a pariah”.
The British HIV Association (BHIVA) has issued a statement on the potential safety signal in infants born to women conceiving on dolutegravir (on behalf of the BHIVA HIV in Pregnancy Guidelines Committee).
The statement reads: “A preliminary unscheduled analysis of an ongoing birth surveillance study in Botswana has reported an increased risk of neural tube defects amongst infants of women who become pregnant whilst taking dolutegravir (DTG)-based regimens. The study reported 4 cases of neural tube defects out of 426 infants born to women who were on DTG-based regimens at the time of conception.
“This rate of approx. 0.9% compares to a 0.1% of neural tube defects amongst infants born to women taking non DTG-based regimens at the time of conception.
“We are awaiting prospective data on 600 women from Botswana and 400 in Brazil who were on DTG-based regimens at conception and have ongoing pregnancies. Of note there have been no reported neural tube defects in infants born to a further 2000 women in the Botswana study who started DTG during pregnancy, including in first trimester.
“In light of these preliminary findings the BHIVA HIV in Pregnancy Guidelines Writing group makes the following recommendations: all women wishing to conceive should be started on folic acid 5mg OD regardless of their cART regimen; all women commencing DTG should have a negative pregnancy test prior to initiation and ongoing method of contraception documented; we advise a review of all patient records of women aged up to 50yo on DTG with regards to conception plans, documented method of contraception and current pregnancy status; and we recommend that women at risk of pregnancy be contacted by their clinic to discuss the DTG safety report, which should be clearly documented, and the woman seen in person if pregnant.
“1. For a woman on DTG wishing to conceive
a. We advise switching to an alternative effective cART regimen
b. The best safety data for pregnancy is for efavirenz or atazanavir/r as per BHIVA HIV in Pregnancy Guidelines 2014
“2. For a woman on DTG not planning children but of child bearing age
a. We advise a discussion on current method of contraception to be clearly documented
“3. For a woman on DTG who becomes or is pregnant
a. We acknowledge the neural tube has closed within 4 weeks of conception but the EMA are recommending that women on DTG in the first trimester discontinue DTG. We therefore recommend that women in the first trimester on DTG switch to a regimen on which there is more safety data in pregnancy, such as efavirenz or atazanavir/r as per BHIVA HIV in Pregnancy Guidelines 2014
b. We do not recommend switching off DTG if in the second or third trimesters
c. If the physician/woman choose(s) to switch, use a regimen on which there is more safety data in pregnancy, such as efavirenz or atazanavir/r as per BHIVA HIV in Pregnancy Guidelines 2014
d. Detailed anomaly scans should be performed as per national pregnancy guidelines with no additional scans required
“4. For a woman who is pregnant and not yet on cART
a. We advise using recommended cART such as efavirenz or atazanair/r as per BHIVA HIV in Pregnancy Guidelines 2014 (currently being updated and due for release this summer) available on www.bhiva.org/guidelines.aspx
“Note that these findings are very preliminary and advice may change. For safety data on antiretrovirals please refer to the Antiviral Pregnancy Registry (www.apregistry.com) or seek advice from an expert colleague.
“This report highlights the need to continue to prospectively report pregnancies to the National Study of HIV in Pregnancy and Childhood (www.ucl.ac.uk/nshpc) and the antiretroviral Pregnancy Registry (www.apregistry.com).”
[link url="https://www.health-e.org.za/2018/05/28/fears-of-birth-defects-prompt-warnings-about-new-hiv-wonder-drug/"]Health-e News report[/link]
[link url="http://www.bhiva.org/BHIVA-statement-on-Dolutegravir.aspx"]BHIVA material[/link]
