Immunotherapy is better than standard “extreme” chemotherapy as first-line treatment for advanced head and neck cancer and can keep some patients alive for more than three years, a major trial reports.
Pembrolizumab either used alone or in combination with chemotherapy was more effective than a standard cocktail of chemotherapy drugs in a study involving nearly 900 patients. For patients who responded to treatment, the duration of response was five times longer for pembrolizumab alone than standard “extreme” chemotherapy
Pembrolizumab now approved in Europe as first-line treatment for patients whose tumours express PD-L1
The immunotherapy drug pembrolizumab alone or in combination with chemotherapy extended patients’ lives compared with standard treatment – with some groups of patients treated with single-agent pembrolizumab responding for five times longer than with standard extreme chemotherapy.
Crucially, the researchers showed it was possible to predict in advance who was more likely to benefit from pembrolizumab by testing for the PD-L1 immune marker in tumours and on surrounding cells – a key step in establishing the drug’s use as a new standard of care.
Pembrolizumab has recently been approved in Europe as first-line treatment for patients diagnosed with advanced head and neck cancer, marking a key milestone in use of immunotherapy as a standard part of cancer treatment.
The phase III trial was led in the UK by The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research, London, and involved 882 patients from all over the world who were diagnosed with advanced head and neck cancer.
The research was funded by the treatment’s manufacturer, Merck, known as MSD outside the US and Canada.
Currently, many patients diagnosed in the UK with advanced head and neck cancer first receive an ‘extreme’ triple combination of two chemotherapies and targeted drug cetuximab.
Another checkpoint inhibitor immunotherapy called nivolumab is available on the NHS via the Cancer Drugs Fund, but only for patients for whom the chemotherapy combination has failed.
But the new trial found that immunotherapy had even more benefit if it’s used as early as possible in treatment for those who are diagnosed with stage III or IV head and neck cancer, when it has begun to or has spread around the body. Around 12,000 people in the UK are diagnosed with head and neck cancer and half will be diagnosed at stage III or IV, so the results could have an impact on a large number of UK patients.
Patients received pembrolizumab combined with chemotherapy, pembrolizumab alone or the extreme combination treatment. Overall, the response rate was 17% with pembrolizumab alone, 36% with standard chemotherapy and 36 per cent with pembrolizumab plus chemotherapy. However, the researchers found that testing for the immune marker PD-L1 in patients’ tumours and surrounding cells could predict who was most likely to respond.
Some 23% of patients who had high levels of PD-L1 in their tumours responded to pembrolizumab alone, and they did so for far longer than chemotherapy – a remarkable average of 23.4 months compared to only 4.5 months in those treated with standard chemotherapy. Even those with moderate levels of PD-L1 responded for 22.6 months.
Many more patients – some 43% – with high levels of PD-L1 responded to immunotherapy plus chemotherapy combination. The average length of response was lower than pembrolizumab alone at 7.1 months, but still 2.6 months longer than standard chemotherapy.
Pembrolizumab alone had a much lower rate of serious side effects, at 55%, than either extreme chemotherapy or pembrolizumab plus chemotherapy (both 85%). Study leader Professor Kevin Harrington, professor of biological cancer therapies at The Institute of Cancer Research, London, and consultant clinical oncologist at The Royal Marsden NHS Foundation Trust, said: “In the last five years immunotherapy has had a big impact on the treatment of many cancers, but generally only after standard treatments such as chemotherapy have failed. Our findings are exciting because they show that immunotherapy could have an even greater impact if used earlier, and in many cases spare patients some of the difficult side effects of chemotherapy.
“Pembrolizumab has been approved both as a single agent and with chemotherapy for advanced head and neck cancer by the US Food and Drug Administration (FDA) and by the European Commission.
“For patients with high levels of the marker PD-L1 whose tumours are smaller and growing relatively slowly, pembrolizumab alone is an excellent treatment option. For patients with larger tumours growing more aggressively, or in those whose tumours express lower levels of the PD-L1 marker, the combination of pembrolizumab and chemotherapy is more likely to be used to get the disease in check.”
This study follows exciting advances in other hard-to-treat cancers, including melanoma. Royal Marsden trials led by Professor James Larkin, whose work is supported by The Royal Marsden Charity, have shown that an immunotherapy combination of drugs called ‘nivolumab’ and ‘ipilimumab’ can have a powerful effect on advanced melanoma. As a result of this research, the drug combination has now become standard practice.
Abstract
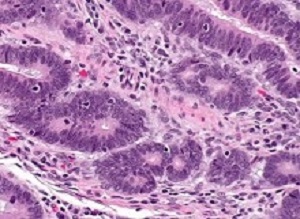
Background: Pembrolizumab is active in head and neck squamous cell carcinoma (HNSCC), with programmed cell death ligand 1 (PD-L1) expression associated with improved response.
Methods: KEYNOTE-048 was a randomised, phase 3 study of participants with untreated locally incurable recurrent or metastatic HNSCC done at 200 sites in 37 countries. Participants were stratified by PD-L1 expression, p16 status, and performance status and randomly allocated (1:1:1) to pembrolizumab alone, pembrolizumab plus a platinum and 5-fluorouracil (pembrolizumab with chemotherapy), or cetuximab plus a platinum and 5-fluorouracil (cetuximab with chemotherapy). Investigators and participants were aware of treatment assignment. Investigators, participants, and representatives of the sponsor were masked to the PD-L1 combined positive score (CPS) results; PD-L1 positivity was not required for study entry. The primary endpoints were overall survival (time from randomisation to death from any cause) and progression-free survival (time from randomisation to radiographically confirmed disease progression or death from any cause, whichever came first) in the intention-to-treat population (all participants randomly allocated to a treatment group). There were 14 primary hypotheses: superiority of pembrolizumab alone and of pembrolizumab with chemotherapy versus cetuximab with chemotherapy for overall survival and progression-free survival in the PD-L1 CPS of 20 or more, CPS of 1 or more, and total populations and non-inferiority (non-inferiority margin: 1·2) of pembrolizumab alone and pembrolizumab with chemotherapy versus cetuximab with chemotherapy for overall survival in the total population. The definitive findings for each hypothesis were obtained when statistical testing was completed for that hypothesis; this occurred at the second interim analysis for 11 hypotheses and at final analysis for three hypotheses. Safety was assessed in the as-treated population (all participants who received at least one dose of allocated treatment). This study is registered at ClinicalTrials.gov, number NCT02358031.
Findings: Between April 20, 2015, and Jan 17, 2017, 882 participants were allocated to receive pembrolizumab alone (n=301), pembrolizumab with chemotherapy (n=281), or cetuximab with chemotherapy (n=300); of these, 754 (85%) had CPS of 1 or more and 381 (43%) had CPS of 20 or more. At the second interim analysis, pembrolizumab alone improved overall survival versus cetuximab with chemotherapy in the CPS of 20 or more population (median 14·9 months vs 10·7 months, hazard ratio [HR] 0·61 [95% CI 0·45–0·83], p=0·0007) and CPS of 1 or more population (12·3 vs 10·3, 0·78 [0·64–0·96], p=0·0086) and was non-inferior in the total population (11·6 vs 10·7, 0·85 [0·71–1·03]). Pembrolizumab with chemotherapy improved overall survival versus cetuximab with chemotherapy in the total population (13·0 months vs 10·7 months, HR 0·77 [95% CI 0·63–0·93], p=0·0034) at the second interim analysis and in the CPS of 20 or more population (14·7 vs 11·0, 0·60 [0·45–0·82], p=0·0004) and CPS of 1 or more population (13·6 vs 10·4, 0·65 [0·53–0·80], p<0·0001) at final analysis. Neither pembrolizumab alone nor pembrolizumab with chemotherapy improved progression-free survival at the second interim analysis. At final analysis, grade 3 or worse all-cause adverse events occurred in 164 (55%) of 300 treated participants in the pembrolizumab alone group, 235 (85%) of 276 in the pembrolizumab with chemotherapy group, and 239 (83%) of 287 in the cetuximab with chemotherapy group. Adverse events led to death in 25 (8%) participants in the pembrolizumab alone group, 32 (12%) in the pembrolizumab with chemotherapy group, and 28 (10%) in the cetuximab with chemotherapy group.
Interpretation: Based on the observed efficacy and safety, pembrolizumab plus platinum and 5-fluorouracil is an appropriate first-line treatment for recurrent or metastatic HNSCC and pembrolizumab monotherapy is an appropriate first-line treatment for PD-L1-positive recurrent or metastatic HNSCC.
Authors
Barbara Burtness, Kevin J Harrington, Richard Greil, Denis Soulières, Makoto Tahara, Gilberto de Castro Jr, Amanda Psyrri, Neus Basté, Prakash Neupane, Åse Bratland, Thorsten Fuereder, Brett G M Hughes, Ricard Mesía, Nuttapong Ngamphaiboon, Tamara Rordorf, Wan Zamaniah Wan Ishak, Ruey-Long Hong, René González Mendoza, Ananya Roy, Yayan Zhang, Burak Gumuscu, Jonathan D Cheng, Fan Jin, Danny Rischin, on behalf of the KEYNOTE-048 Investigators
Cases of head and neck cancers are rising in the UK and most are diagnosed late, when they are hard to treat, says a BBC News report. Derek Kitcherside, 70, from Leicestershire, believes he wouldn't be here without pembrolizumab. He was diagnosed with cancer of the voice-box in 2011. When he started coughing up blood three years later, after receiving standard treatment, he was told the cancer had spread to his lungs and was probably incurable.
Derek asked to go on a drug trial and travelled to London every three weeks for two years for treatment with pembrolizumab. "My tumour was shrinking all the time and I felt a bit better every time I went," he said. "It made a huge difference to my life." Regular scans show the disease is now stable and the tumour is still getting smaller. "I'm very pleased I can get on with my life," Derek said. "I don't think I'd be here without it."
Pembrolizumab is already being used to treat a wide range of advanced cancers, including melanoma – a type of skin cancer that spreads easily. Experts believe the drug has the potential to treat many more.
"This study is very exciting", says Professor Paul Workman, from the Institute of Cancer Research. "Firstly, because it shows that immunotherapy can have dramatic benefits for some patients with head and neck cancer when used as a first-line treatment, and secondly because the researchers have devised a test for picking out who is most likely to benefit."
He said all new drugs coming on to the market should be accompanied by a test to target their uses as precisely as possible. In the US and the EU, pembrolizumab has been approved for use on its own and with chemotherapy for advanced head and neck cancer, but not yet in the UK.
The report says the National Institute for Heath-Care and Excellence is currently appraising pembrolizumab and it could be approved for use on the NHS by next summer.
[link url="https://www.royalmarsden.nhs.uk/major-trial-backs-immunotherapy-standard-first-line-treatment-head-and-neck-cancer"]Royal Marsden NHS Hospital Trust material[/link]
[link url="https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(19)32591-7/fulltext"]The Lancet abstract[/link]
[link url="https://www.bbc.com/news/health-50507069"]BBC News report[/link]