Even as BA.4 and BA.5 continue to climb the charts, crowding out earlier Omicron subvariants, scientists are warning about an even newer strain: BA.2.75. At this stage, however, they say it’s too early to tell how deadly or virulent it might be.
Tom Peacock, PhD, a virologist at Imperial College London, tweeted on 30 June, “worth keeping a close eye on BA.2.75 – lots of spike mutations, probable second generation variant, apparent rapid growth and wide geographical spread” reports MedPage Today.
It’s a fast spreading variant with a host of spike mutations appearing together, but scientists say it’s still too soon to know for certain exactly how much better – if at all – BA.2.75 is at escaping natural and vaccine-induced immunity.
Here’s what we know so far about the newly mutated descendent of BA.2:
Where is it spreading?
So far, the subvariant has made its way to at least 10 countries in Asia, Europe, North America and Australia.
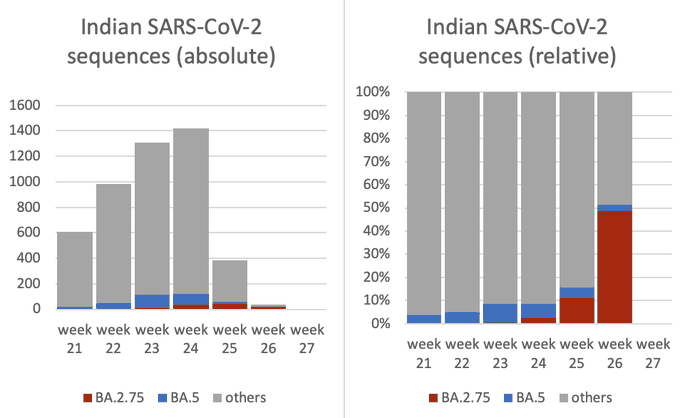
BA.2.75 was first detected in India in early May and has been spreading quickly since. It comprised almost 25% of samples there as of 2 June and is competing with BA.5 and BA.2, according to Katelyn Jetelina, PhD, MPH, an epidemiologist at the University of Texas School of Public Health in Dallas.
A more recent analysis of coronavirus sequencing, posted by a scientist in Australia, suggested the proportion of cases has jumped much higher as at 8 July – growing to nearly half of COVID cases sequenced in India.
A Centres for Disease Control and Prevention (CDC) spokesperson confirmed to MedPage Today that there have been two cases of BA.2.75 detected in the US, with the first specimen collected on 14 June. This is still not enough to get on the CDC’s variant tracker, where it is still unlisted.
Is it more transmissible?
The BA.2.75 lineage has “nine unique changes in the spike protein”, according to a Twitter thread from Vinod Scaria, MBBS, PhD, principal scientist at the CSIR Institute of Genomics & Integrative Biology in New Delhi.
One mutation, G446S, is in the part of the spike protein that binds to receptors in our human cells, and is “associated with major immune (Ab) escape”.
Scaria also said while the number of genomes available to examine in India is still very small, “the rapid increase in recent weeks … suggests it might have a growth advantage”.
However, Marc Johnson, PhD, a professor of molecular microbiology and immunology at the University of Missouri’s school of medicine, told MedPage Today that “we don’t really know if BA.2.75 is more transmissible or more severe at this point”.
“What we do know is that it has amino acid changes that allow it to evade particular neutralising antibodies,” he added.
Is it more severe?
Johnson and Scaria said there is not yet any suggestion that BA.2.75 is more virulent or will increase mortality.
The WHO’s chief scientist, Dr Soumya Swaminathan, said “it’s still too early to know if this subvariant has properties of additional immune invasion, or indeed of being more clinically severe”.
However, Jetelina noted that a recent analysis suggested “BA.2.75’s impact will be dependent on infection history”, and that those with a previous BA.1 infection may actually have a lower probability of losing immunity than those who had BA.2.
Will vaccines and treatments provide protection?
As with each subvariant removed from the ancestral strains of SARS-CoV-2 on which the jabs were based, “vaccines will still provide protection [against BA.2.75], but even less than before”, Johnson said. However, it’s important to note that vaccines still offer strong protection against severe COVID-19 disease and death.
“Given the additional mutations, it is likely nearly all monoclonal antibodies are ineffective against BA.2.75, as is the case for BA.5,” Dr Charles Chiu, PhD, a professor of laboratory medicine and infectious diseases at the University of California San Francisco, told MedPage Today. But he noted that oral antivirals like nirmatrelvir-ritonavir (Paxlovid) have continued to be effective in treating Omicron sublineages.
Is there reason for concern?
“We should be concerned, yes, but we shouldn’t freak out,” Johnson said. “This lineage has a good chance to increase infections and become the new dominant lineage, but it is not likely to cause a sweeping wave the way Omicron did.”
Scientists said much more genomic surveillance and data are needed to gain a more complete picture, and Peacock wrote that BA.2.75 might not even grow to be a dominant force.
“It’s entirely possible this is just growing against a background of BA.2 (.12.1) and that it hits the encroaching wall of BA.5 and stalls out,” he tweeted.
In April this year, BA.4 and BA.5 Omicron sub-variants led to a small spike in cases in South Africa, causing an “unofficial” fifth wave.
Speaking to IoL News at the time, infectious diseases expert at the KwaZulu-Natal Research Innovation and Sequencing Platform (KRISP) Dr Richard Lessells said it is normal for COVID-19 variants to have multiple different sub-lineages.
“Delta now has 133 sub-lineages (AY.1 to AY.133) according to the same definitions. So we do fully expect to see more Omicron sub-lineages over time,” he said.
IoL article – WHO monitors new sub-variant of Omicron BA.2.75 first detected in India (Open access)
See more from MedicalBrief archives:
NICD statistics: COVID cases rise as two Omicron sub-lineages spread across SA
Omicron sub-variant BA.2 warning for US as European cases surge
Tests and wastewater analyses signal a possible 5th wave in SA
Pfizer-BioNTech vaccine holds up against Omicron – Discovery analysis
