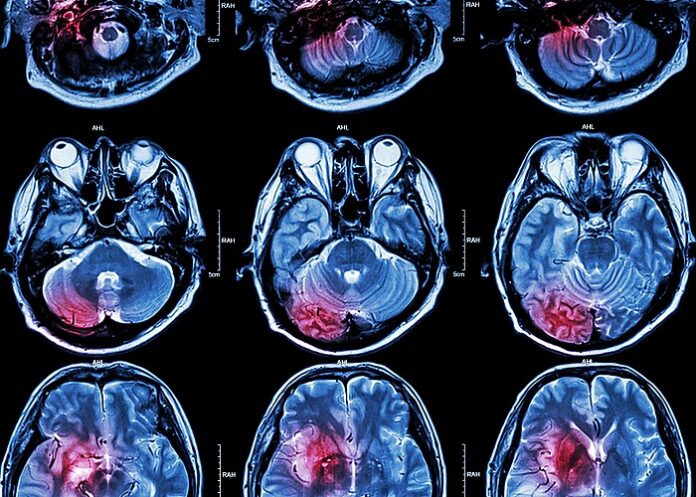
Patients with COVID-19 who suffer acute ischaemic stroke (AIS) appear to be at significantly higher risk of severe disability and death compared with stroke patients treated in the pre-COVID era, found a multicentre US study.
Numerous clinicians from stroke centres across the US and Canada have reported that a third of all patients with COVID-19 may develop neurological complications from infection, and suffer
Massachusetts General Hospital (MGH) and 29 other stroke centres say that patients with COVID-19 who experience AIS appear to be at higher risk of severe disability and death compared with stroke patients treated in the pre-COVID era.
Dr Adam Dmytriw, an interventional neuroradiology and endovascular neurosurgery fellow at MGH, and colleagues, looked at records of 230 patients with AIS who were seen at the stroke centres during the first wave of the pandemic, from mid-March until the end of August 2020.
As they reported in the Journal of Neurology, Neurosurgery & Psychiatry, slightly more than half (51%) of all patients had poor outcomes, with 39,1% dying either in hospital or within 30 days of being discharged. In contrast, data from large clinical trials conducted before the pandemic show death rates of 27,6% among all patients with ischaemic strokes, and 11, 6% among patients with strokes caused by blockage of one or more large blood vessels that supply blood to much of the brain.
“There is an interaction that is still unknown between COVID respiratory disease and stroke, because the rate of poor outcomes or mortality is clearly greater than it would be in someone who had just an acute respiratory distress syndrome or COVID pneumonia, and also worse than someone who would have an equivalently large stroke in the pre-COVID era,” said Dmytriw.
The still-growing North American Neurovascular COVID-19 (NAN-C) Consortium was founded by Dmytriw in collaboration with centres in New York and is supervised by Dr Aman Patel and Dr Robert Regenhardt, at MGH. The hospitals participating in the study represent a broad spectrum of stroke centres with patients from a variety of socioeconomic backgrounds and varying access to care, Dmytriw notes.
“This study is something of a post-mortem of how the hardest hit areas responded to the first wave of the pandemic,” he said. “Some of the initial reports we had came from hospitals in more affluent areas, such as central Manhattan where people with lower socioeconomic status were less likely to present. Even though Mass General is one such hospital, our goal was to create a consortium including hospitals in outer boroughs of New York, outside the greater Boston area, within and around Detroit, as well as diverse centres from coast to coast.
“The study revealed how great the mortality was from COVID-associated stroke during the first wave, how high the rates of disability were for many patients, and that these mortality rates and disabilities were greater than those experienced in the first wave in other countries,” he said.
The data suggest that patients from less affluent areas may have been at greater risk of serious complications such as stroke because of their inability to carry out protective measures likes social distancing or working at home, he added.
Study details
Acute ischaemic stroke associated with SARS-CoV-2 infection in North America
Adam Dmytriw, Mahmoud Dibas, Kevin Phan, Aslan Efendizade, Johanna Ospel, Clemens Schirmer, Fabio Settecase, Manraj Heran, Anna Luisa Kühn, Ajit Puri, Bijoy Menon, Sanjeev Sivakumar, Askan Mowla, Daniel Vela-Duarte, Italo Linfante, Guilherme Dabus, Robert Regenhardt, Salvatore D'Amato, Joseph Rosenthal, Alicia Zha, Nafee Talukder, Sunil Sheth, Ameer Hassan, Daniel Cooke, Lester Leung, Adel Malek, Barbara Voetsch, Siddharth Sehgal, Ajay Wakhloo, Mayank Goyal, Hannah Wu, Jake Cohen, Sherief Ghozy, David Turkel-Parella, Zerwa Farooq, Justin Vranic, James Rabinov, Christopher Stapleton, Ramandeep Minhas, Vinodkumar Velayudhan, Zeshan Ahmed Chaudhry, Andrew Xavier, Maria Bres Bullrich, Sachin Pandey, Luciano Sposato, Stephen Johnson, Gaurav Gupta, Priyank Khandelwal, Latisha Ali, David Liebeskind, Mudassir Farooqui, Santiago Ortega-Gutierrez, Fadi Nahab, Dinesh Jillella, Karen Chen, Mohammad Ali Aziz-Sultan, Mohamad Abdalkader, Artem Kaliaev, Thanh Nguyen, Diogo Haussen, Raul Nogueira, Israr Ul Haq, Osama Zaidat, Emma Sanborn, Thabele Leslie-Mazwi, Aman Patel, James Siegler, Ambooj Tiwari.
Published in the Journal of Neurology, Neurosurgery & Psychiatry on 7 February 2022
Abstract
Background
To analyse the clinical characteristics of COVID-19 with acute ischaemic stroke (AIS) and identify factors predicting functional outcome.
Methods
Multicentre retrospective cohort study of COVID-19 patients with AIS who presented to 30 stroke centres in the USA and Canada between 14 March and 30 August 2020. The primary endpoint was poor functional outcome, defined as a modified Rankin Scale (mRS) of 5 or 6 at discharge. Secondary endpoints include favourable outcome (mRS ≤2) and mortality at discharge, ordinal mRS (shift analysis), symptomatic intracranial haemorrhage (sICH) and occurrence of in-hospital complications.
Results
A total of 230 COVID-19 patients with AIS were included. 67.0% (154/230) were older than 60 years, while 33.0% (76/230) were younger. Median (IQR) National Institutes of Health Stroke Scale (NIHSS) at presentation was 12.0 (17.0) and 42.8% (89/208) presented with large vessel occlusion (LVO). Approximately 50.2% (102/203) of the patients had poor outcomes with an observed mortality rate of 38.8% (35/219). Age >60 years (aOR: 4.60, 95% CI 1.89 to 12.15, p=0.001), diabetes mellitus (aOR: 2.53, 95% CI 1.14 to 5.79, p=0.025), increased NIHSS at admission (aOR: 1.10, 95% CI 1.05 to 1.16, p<0.001), LVO (aOR: 3.02, 95% CI 1.27 to 7.44, p=0.014) and no IV tPA (aOR: 2.76, 95% CI 1.06 to 7.64, p=0.043) were significantly associated with poor functional outcome.
Conclusion
There may be a relationship between COVID-19 associated AIS and severe disability or death. We identified several factors that predict worse outcomes, and these outcomes were more frequent compared with global averages. We found that elevated neutrophil-to-lymphocyte ratio, rather than D-dimer, predicted both morbidity and mortality.
See more from MedicalBrief archives:
COVID-19 increases acute myocardial infarction and ischaemic stroke risk
Stroke risk higher than expected among COVID-19 patients
Increased risk of death and serious illness among COVID-19 survivors
Preliminary results from two UK studies suggest significant heart inflammation from COVID
COVID-19 patients with neurological symptoms have 6x higher hospital mortality