Despite South Africa producing a substantial number of trained optometrists, most of them work in the private sector and in urban areas, an imbalance that leaves rural communities underserved, and exacerbates health inequities.
So does it make sense to use public funds and institutions to train people predominantly for the private sector, ask Dr Haseena Majid and Rene Sparks, writing in Spotlight.
Avoidable blindness and vision impairment are major global health concerns. The WHO estimates that at least 1bn people worldwide have a vision impairment that could have been prevented or treated.
In 2020, around 11m people had some degree of vision loss in South Africa, of whom 370 000 were classified as blind.
Avoidable blindness caused by uncorrected refractive error (vision problems that requires spectacles or contact lenses) and cataracts can be well managed by a capable work force that is both accessible and affordable to the public.
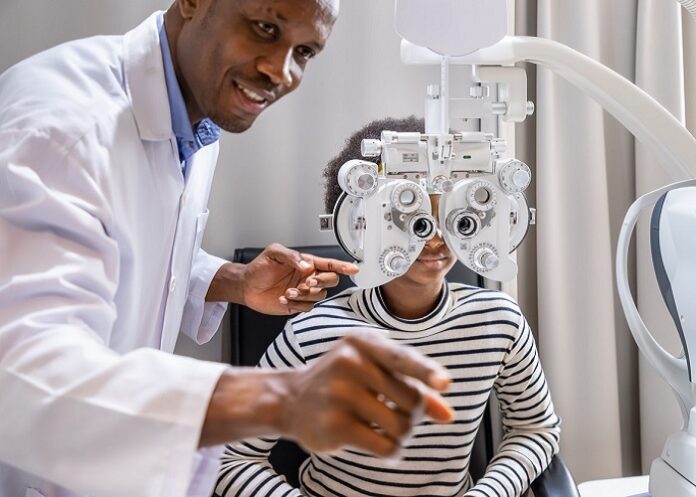
As such, optometrists are crucial in combating avoidable vision loss.
Their expertise in conducting comprehensive eye examinations, diagnosing and managing some eye diseases, prescribing corrective lenses, and providing preventive care, is vital for reducing the burden of avoidable blindness.
But the current landscape of optometry services in this country reveals significant gaps in both governance and resource allocation.
The distribution of optometrists in South Africa is far from optimal. In April 2023, there were around 4 200 registered optometrists and 580 ophthalmologists in the country. While this is a considerable number of people trained to provide primary eye care services, the 6.7% serving the public sector – compared with 93.3% serving the private sector – is simply inadequate and has created stark disparities.
The available evidence points to an urban-rural divide in optometry services, with only around 262 optometrists employed by the state nationally, and disproportionately between and within provinces. It means that rural and poor communities, where a significant portion of the population lives, have very limited access to essential eye care services.
Further deepening the disparities is the government’s fragmented and inconsistent approach to eye health across provinces, resulting in some areas lacking any public eye care services, while others depend on external providers.
Training misalignment
All of these challenges come against the backdrop of substantial state investment in the training of optometrists. The government funds their training at several universities countrywide. However, most of these graduates are absorbed into the private sector. In some instances, students trained on state bursaries struggle for jobs in the public sector.
This misalignment highlights a fundamental flaw in how public funds are utilised, with minimal benefit to the broader population that relies on public healthcare. It also contradicts the government’s mandate to provide progressive solutions to improve access to healthcare for all, as enshrined in the Constitution.
These ongoing governance gaps and the inefficient use of state resources also represent significant barriers to achieving health equity in South Africa as expressed in government’s plans for National Health Insurance (NHI).
And while the implementation of NHI aims to bring our country closer towards universal health coverage, it is not yet clear whether, and to what extent, vision and eye care services will be included in the envisioned basket of services.
A lack of a clear plan could result in a missed opportunity to integrate optometrists into the primary healthcare system nationally.
What to do
First, there needs to be an urgent reassessment of the costs to train optometrists against the benefits to the broader public. Are we training too many optometrists? Could the government initiate engagements with thought leaders and support partners to develop a community service and costing exercise to address the inequity and lack of access to eye health services, and simultaneously tackle the employment of optometrists within the public health space?
Second, the National Department of Health should establish a dedicated directorate for eye health services, which should be integrated within provincial health structures. This unit should spearhead a comprehensive data collection system for vision and eye health that could be used to accurately assess needs, allocate resources, and plan effectively.
Calls for such a dedicated directorate have been made through scientific recommendation for more than a decade. But there has been no meaningful response and action from the Health Department and related decision-making entities.
Third, the principles behind NHI offer a medium-term solution to address the disproportionate distribution of optometrists. Through the establishment of NHI-style public-private partnerships, private sector capacity can be leveraged to serve people who depend on the public sector.
Such a partnership will require transparency, accountability, and data integrity built into its structures. This will allow provinces and districts to monitor accurate data, and provide feedback to help shape and improve services.
In summary, the Health Department stands at a critical juncture, where the systemic imbalances in optometrist distribution and vision care services have now become acute – with South Africans paying a very concrete and personal price in the form of avoidable vision loss.
Delays in governance processes have historically hampered progress, but the need for swift and informed action is paramount.
The principles of public-private partnership that underlie NHI point to a solution, but the urgency of the crisis means we do not have the time to wait for the full NHI plans to be rolled out – by government’s own admission that will take many years. People losing their eyesight today simply can’t wait that long.
*Majid and Sparks are Global Atlantic fellows for Health Equity in South Africa and advocates on the National Eye Health Advocacy Project led by USAWA for learning and healing, a civil society organisation committed to reforms for health equity and social justice.
See more from MedicalBrief archives:
KZN Health defends its capacity to perform eye surgery
Many ophthalmologists are missing AMD indicators
Chiropractic neck manipulation and vision loss