 A ground-breaking Loyola Medicine study suggests that a simple 15-minute electrocardiogram could help a physician determine whether a patient has major depression or bipolar disorder.
A ground-breaking Loyola Medicine study suggests that a simple 15-minute electrocardiogram could help a physician determine whether a patient has major depression or bipolar disorder.
Bipolar disorder often is misdiagnosed as major depression. But while the symptoms of the depressive phase of bipolar disorder are similar to that of major depression, the treatments are different and often challenging for the physician.
In bipolar disorder, formerly called manic depression, a patient swings between an emotional high (manic episode) and severe depression. Treatment for the depressed phase includes an antidepressant along with a safeguard such as a mood stabiliser or anti-psychotic drug to prevent a switch to a manic episode. A physician who misdiagnoses bipolar disorder as major depression could inadvertently trigger a manic episode by prescribing an antidepressant without a safeguard mood stabilising drug.
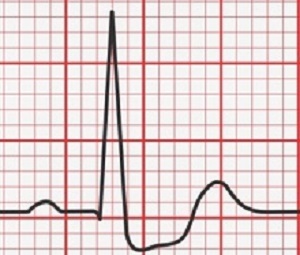
The study found that heart rate variability, as measured by an electrocardiogram, indicated whether subjects had major depression or bipolar disorder. (Heart rate variability is a variation in the time interval between heartbeats.) The stud was led by senior author Dr Angelos Halaris.
"Having a non-invasive, easy-to-use and affordable test to differentiate between major depression and bipolar disorder would be a major breakthrough in both psychiatric and primary care practices," Halaris said. Halaris said further research is needed to confirm the study's findings and determine their clinical significance.
Halaris is a professor in Loyola's department of psychiatry and behavioural neurosciences and medical director of adult psychiatry.
Major depression is among the most common and severe health problems in the world. In the US, at least 8% to 10% of the population suffers from major depression at any given time. While less common than major depression, bipolar disorder is a significant mental health problem, affecting an estimated 50m people worldwide.
The Loyola study enrolled 64 adults with major depression and 37 adults with bipolar disorder. All subjects underwent electrocardiograms at the start of the study. Each participant rested comfortably on an exam table while a three-lead electrocardiogram was attached to the chest. After the patient rested for 15 minutes, the electrocardiographic data were collected for 15 minutes.
Using a special software package, researchers converted the electrocardiographic data into the components of heart rate variability. These data were further corrected with specialised software programs developed by study co-author Dr Stephen W Porges, of Indiana University's Kinsey Institute.
In measuring heart rate variability, researchers computed what is known to cardiologists as respiratory sinus arrhythmia (RSA). At the baseline (beginning of the study), the subjects with major depression had significantly higher RSA than those with bipolar disorder.
In a secondary finding, researchers found that patients with bipolar disorder had higher blood levels of inflammation biomarkers than patients with major depression. Inflammation occurs when the immune system revs up in response to a stressful condition such as bipolar disorder.
Abstract
Objectives: Major depressive disorder (MDD) and depression in bipolar disorder (BD) are often difficult to distinguish from each other. Autonomic nervous system (ANS) dysregulation is associated with various depressive symptoms and inflammatory response disinhibition. The beat-to-beat pattern of heart rate (heart rate variability, HRV) offers a non-invasive portal to ANS function and provides a reliable index of resting cardiac vagal tone. We quantified HRV and measured inflammatory biomarkers in MDD and BD patients in an effort to derive potential diagnostic criteria for MDD and BD.
Methods: Sixty-four MDD and 37 BD patients were enrolled. HRV was assessed and blood was drawn at baseline after antidepressant washout and prior to study initiation. HRV was quantified and corrected for artefacts.
Results: MDD subjects had significantly higher baseline respiratory sinus arrhythmia (P = 0.05) and LF-HRV (P < 0.01) in comparison to BD subjects. Compared to MDD subjects, BD subjects had significantly higher baseline levels of IL-10 (P < 0.01) and MCP-1 (P < 0.01). In the MDD group only, baseline LF-HRV was significantly positively correlated to baseline levels of IL-10 (r = 0.47, P < 0.01).
Conclusions: Reduced vagal tone and higher levels of inflammatory biomarkers may distinguish BD from MDD and reveal an underlying pathophysiology of depression involving ANS dysfunction and chronic immune system dysregulation.
Authors
Brandon Hage, Briana Britton, David Daniels, Keri Heilman, Stephen W Porges, Angelos Halaris
[link url="https://www.sciencedaily.com/releases/2017/11/171121095403.htm"]Loyola University Health System material[/link]
[link url="http://www.tandfonline.com/doi/full/10.1080/15622975.2017.1376113"]The World Journal of Biological Psychiatry abstract[/link]
