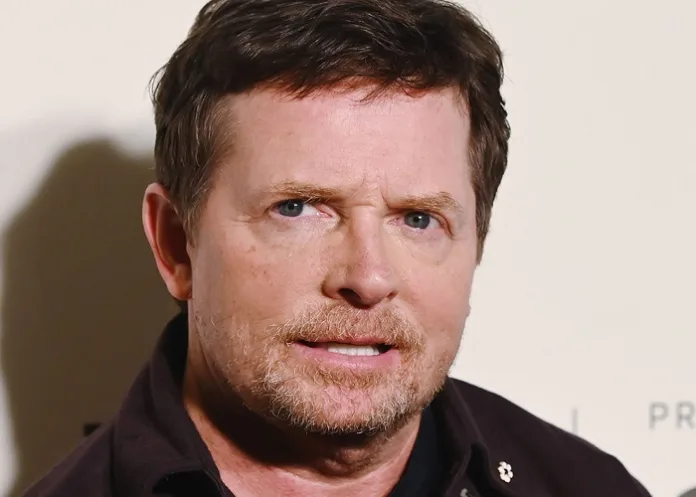
Research funded by former film star and Parkinson’s sufferer Michael J Fox has resulted in the clearest evidence yet that the presence of a particular misfolded protein, alpha-synuclein, can determine if people have the disease or not – an advance that may soon be used to develop better diagnostics, and that could also rapidly accelerate the search for treatments.
The findings of the research – funded by the Michael J Fox Foundation for Parkinson’s Research and published in The Lancet Neurology – are the result of a 1 123-person study that has cost the foundation hundreds of millions of dollars since it began in 2010.
Right now, alpha-synuclein can only be detected by taking a spinal tap, a difficult and uncomfortable procedure, notes STAT News. But scientists hoped it could be detected in blood, a skin biopsy, or possibly even in a swab of the nose. An editorial in the medical journal called the test “a game-changer in Parkinson’s disease diagnostics, research, and treatment trials”.
The result is convincing in part because of the unique resource of patient volunteers Fox was able to bring together, said Vikram Khurana, chair of movement disorders at Brigham & Women’s Hospital.
“It is head and shoulders… the best resource we have in the Parkinson’s disease research community to really analyse the behaviour and molecular and clinical aspects of our patients,” Khurana said.
Fox, who was diagnosed with Parkinson’s at 29, said he keeps going back to documentary footage of his childhood. Then, there was no way to know he would develop the disease; soon, he said, a child like that might be able to simply get a nasal swab at two or three or four-years-old. “It’s all changed. It can be known and treated early on. It’s huge.”
There is still a long way to go before people can be screened this way. And using the new discovery to craft better drug trials and speed treatments to market could take a decade although the Fox Foundation, always optimistic, believes it can do the work in three to five years. But Fox sees the result as the biggest victory yet in a battle that has taken decades and billions of donated dollars.
It’s a battle he feels ready to wage.
Fox moved from Canada to the US when he was 16, and turned dumpster diving and landlord ducking into a series, to become one of the biggest movie stars in the world. The series was Family Ties, on the set of which he met his wife of 34 years, Tracy Pollan. He also starred in Back to the Future and its sequels, all of them blockbusters.
But in 1991 he was diagnosed with Parkinson’s. For seven years he hid the condition, but in 1998 he went public. “I had to tell people,” he said. “They were going to notice.”
He launched the Fox Foundation and threw himself into the effort almost completely: he also had an amazing ability to pull in both top scientists and big donors.
As CEO, Fox recruited Deborah Brooks, a Goldman Sachs banker, who remains in the role today. (For a time, she stepped back as executive chairwoman). Among their earliest advisers was Andrew Grove, the former CEO of Intel, who also had Parkinson’s.
The idea for the current study, called the Parkinson’s Progression Markers Initiative, came in 2008. The idea was to follow patients whose Parkinson’s was diagnosed in the earlier stages of the disease, to better understand how the disease progressed. It was clear from the start the project would take many years and plenty of money.
Todd Sherer, who took over for Brooks as CEO for a time and is currently the foundation’s chief mission officer, said relying on animal systems was part of what was holding Parkinson’s research back. It was better, he argued, to look at what actually happened in people, even if doing so would be difficult and expensive.
At that point, the foundation had funded perhaps $25m of biomarker research. The new study, it was thought, would cost $15m a year.
Brooks remembers that when this idea was taken to the board, many asked why it was a key priority. And if the study would make it easier for pharmaceutical companies to fund research, why weren’t they funding it.
“Ultimately it was Michael,” Brooks recalled. “He leaned over in the board meeting and said, ‘I don’t know the details. But it sounds like this is something that has to be done. If it’s not us, who?’”
Between 7 July 2010, and 4 July 2019, the study signed up 1 123 patients. Of these, 545 had Parkinson’s disease, 163 were healthy people with no evidence of Parkinson’s disease, 54 had evidence of the disease on brain scans, 51 were in the early stages of the disease, and 310 had genetic mutations that should cause Parkinson’s but hadn’t yet done so.
Whether the presence of alpha-synuclein could signal Parkinson’s early was an obvious question. The protein accumulates in clumps in the brain, known as Lewy bodies – a hallmark of both Parkinson’s and another disorder, Lewy body dementia. A genetic mutation related to alpha-synuclein was shown to cause Parkinson’s in a study of Greek and Italian patients in 1997.
The results were stunning. Using synuclein as a test in early Parkinson’s detected the disease 87% of the time. What’s more, in volunteers who did not have Parkinson’s, the test showed the absence of the disease 96% of the time.
“This changes things in many ways in a positive direction,” said Ken Marek, president of the Institute for Neurodegenerative Disorders and principal investigator of the PPMI study. “It enables us to be more clear for individuals who might have or who have what we now think of as Parkinson’s disease.”
One of the big surprises was that not all patients had the same biology. For instance, mutations in one particular gene, known as LRRK2, were known to cause Parkinson’s.
One of the more promising experimental drugs against Parkinson’s, which is being developed by the biotech firm Denali Therapeutics, is being tested particularly in people with the LRRK2 mutation.
Yet 30% of people with the LRRK2 mutation, which causes a disease that looks like Parkinson’s, do not have alpha-synuclein. They appear to have a different biological disease, Marek said. Meanwhile, in another group – those who have lost their sense of smell, which is a hallmark of Parkinson’s – the test detected the disease 98.6% of the time.
Those differences, Marek said, could be a key clue to treating Parkinson’s. Perhaps an LRRK2 drug works in the people who have synuclein – in Marek’s formulation, who have Parkinson’s. Until now, it was not clear that researchers should look.
Carole Ho, chief medical officer of Denali, which is testing a medicine that targets LRRK2, disagreed that LRRK2 patients have something other than Parkinson’s. She also said it was known Parkinson’s patients with this condition do not always have measurable alpha-synuclein. Khurana, the Brigham and Women’s researcher, said that seeing such definitive numbers would still have an impact on the field.
In the near term, Marek said, the result will have practical implications for cases in which doctors are not sure if they are dealing with Parkinson’s or not. A commercial test is already available. Testing whether the assay can be used for screening will take longer, and involve learning how to test for levels of synuclein in blood, skin, or on nasal swabs.
“This is the newest chapter, and one in which we got something done, something that is fundamentally going to change the world,” Fox said. “I don’t say that lightly. I don’t say it with any credit. It’s the way it worked out.”
That, he added, could “open the floodgates”. The Fox Foundation is already beginning studies to use DNA sequencing data collected from these patients to understand how different genes might affect Parkinson’s progression.
Another target will be to see if instead of just viewing alpha synuclein as an on-off switch, researchers can check levels of the protein to determine how advanced Parkinson’s is and even to see if drugs can lower the protein’s concentrations.
Outside researchers and drug industry experts agree with that potential, but also see big hurdles to reaching it. Showing the assay can work is a “tour de force”, said neurologist David Eidelberg from the Feinstein Institutes for Medical Research.
But what’s not clear is how quickly someone who tests positive for alpha-synuclein will develop Parkinson’s. Will it be months or years? The lack of that information will make it more difficult to use the test to design clinical trials.
Still, the existence of a test makes possible studies that would not have been possible before. Ho, the Denali executive, said it was now possible to conduct trials early in the disease. “This is the first time there’s been an identification of a biochemical assay that can predict the likelihood of somebody having Parkinson’s,” she said.
Frank D’Amelio, who was the chief financial officer of Pfizer for 15 years, recently joined the Fox Foundation’s board. “Hopefully this could lead to better clinical trial design, faster clinical trial execution, and hopefully at some point medicines that can actually slow down the disease’s progression.”
In turn, that could make Parkinson’s a more appealing disease for drug companies to target, because faster trials means treatments are on the market longer before their patents expire.
Many researchers said that they hoped the research would be similar to Alzheimer’s, where the ability to identify patients with particular abnormal peptides has led to drugs that have at least some efficacy against the disease.
Study details
Assessment of heterogeneity among participants in the Parkinson's Progression Markers Initiative cohort using α-synuclein seed amplification: a cross-sectional study
Andrew Siderowf, Luis Concha-Marambio, David-Erick Lafontant, Carly Farris, Yihua Ma, Paula Urenia, et al.
Published in The Lancet Neurology in May 2023
Summary
Background
Emerging evidence shows that α-synuclein seed amplification assays (SAAs) have the potential to differentiate people with Parkinson's disease from healthy controls. We used the well characterised, multicentre Parkinson's Progression Markers Initiative (PPMI) cohort to further assess the diagnostic performance of the α-synuclein SAA and to examine whether the assay identifies heterogeneity among patients and enables the early identification of at-risk groups.
Methods
This cross-sectional analysis is based on assessments done at enrolment for PPMI participants (including people with sporadic Parkinson's disease from LRRK2 and GBA variants, healthy controls, prodromal individuals with either rapid eye movement sleep behaviour disorder (RBD) or hyposmia, and non-manifesting carriers of LRRK2 and GBA variants) from 33 participating academic neurology outpatient practices worldwide (in Austria, Canada, France, Germany, Greece, Israel, Italy, the Netherlands, Norway, Spain, the UK, and the USA). α-synuclein SAA analysis of CSF was performed using previously described methods. We assessed the sensitivity and specificity of the α-synuclein SAA in participants with Parkinson's disease and healthy controls, including subgroups based on genetic and clinical features. We established the frequency of positive α-synuclein SAA results in prodromal participants (RBD and hyposmia) and non-manifesting carriers of genetic variants associated with Parkinson's disease, and compared α-synuclein SAA to clinical measures and other biomarkers. We used odds ratio estimates with 95% CIs to measure the association between α-synuclein SAA status and categorical measures, and two-sample 95% CIs from the resampling method to assess differences in medians between α-synuclein SAA positive and negative participants for continuous measures. A linear regression model was used to control for potential confounders such as age and sex.
Findings
This analysis included 1123 participants who were enrolled between July 7, 2010, and July 4, 2019. Of these, 545 had Parkinson's disease, 163 were healthy controls, 54 were participants with scans without evidence of dopaminergic deficit, 51 were prodromal participants, and 310 were non-manifesting carriers. Sensitivity for Parkinson's disease was 87·7% (95% CI 84·9–90·5), and specificity for healthy controls was 96·3% (93·4–99·2). The sensitivity of the α-synuclein SAA in sporadic Parkinson's disease with the typical olfactory deficit was 98·6% (96·4–99·4). The proportion of positive α-synuclein SAA was lower than this figure in subgroups including LRRK2 Parkinson's disease (67·5% [59·2–75·8]) and participants with sporadic Parkinson's disease without olfactory deficit (78·3% [69·8–86·7]). Participants with LRRK2 variant and normal olfaction had an even lower α-synuclein SAA positivity rate (34·7% [21·4–48·0]). Among prodromal and at-risk groups, 44 (86%) of 51 of participants with RBD or hyposmia had positive α-synuclein SAA (16 of 18 with hyposmia, and 28 of 33 with RBD). 25 (8%) of 310 non-manifesting carriers (14 of 159 [9%] LRRK2 and 11 of 151 [7%] GBA) were positive.
Interpretation
This study represents the largest analysis so far of the α-synuclein SAA for the biochemical diagnosis of Parkinson's disease. Our results show that the assay classifies people with Parkinson's disease with high sensitivity and specificity, provides information about molecular heterogeneity, and detects prodromal individuals before diagnosis. These findings suggest a crucial role for the α-synuclein SAA in therapeutic development, both to identify pathologically defined subgroups of people with Parkinson’s disease and to establish biomarker-defined at-risk cohorts.
See more from MedicalBrief archives:
Prostate drug associated with lower risk of Parkinson’s — large international analysis
Visual dysfunction predicts Parkinson’s-linked cognitive decline 18 months ahead
Thousands of Parkinson’s patients initially misdiagnosed
Small pioneering study offers hope to Parkinson’s patients
Big data, lab science suggests drug may slow Parkinson’s progression in people