More than half of people living with HIV and suppressed viral loads nonetheless had imaging-confirmed coronary artery disease. But despite long-time use of HIV drugs associated with cardiovascular trouble, none of those drugs was implicated in disease risk, according to research presented at the 18th European AIDS Conference.
“Traditional risk factors and duration of HIV infection was associated with severe coronary artery disease,” said Dr Andreas Knudsen, an infectious disease provider at Copenhagen University Hospital, Hvidovre, Denmark, during his presentation. “When we adjusted for time since diagnosis of HIV, none of the drugs remained associated with the severity of coronary artery disease.”
Notably, that included abacavir, which was found in another EACS presentation and in past research to be associated with increased rates of heart attacks. Abacavir is sold individually as a generic as well as a component of Epzicom (abacavir/lamivudine) and the single-drug regimen Triumeq (dolutegravir/abacavir/lamivudine).
The Copenhagen Comorbidity in HIV Infection (COCOMO) study enrolled 1,099 people living with HIV in the Danish capital beginning in 2015, and 705 of them had angiographies via CT available to include in the results. Participants were mainly male (89%), at a healthy weight (BMI of 25), and 96% had undetectable viral loads.
Large minorities of participants also had traditional risk factors for coronary artery disease. More than one in four smoked, one in five had high cholesterol, and 42% had high blood pressure. In addition, many had used drugs associated with cardiovascular trouble, including abacavir, used by 26% of participants; indinavir, used by 17%; zidovudine/AZT, used by 47%; and didanosine, used by 14%.
(While abacavir is still in use, the other three drugs are considered legacy drugs and are not in current use.)
In addition, nearly one in three (29%) was currently using a protease inhibitor, which has been associated with heart failure.
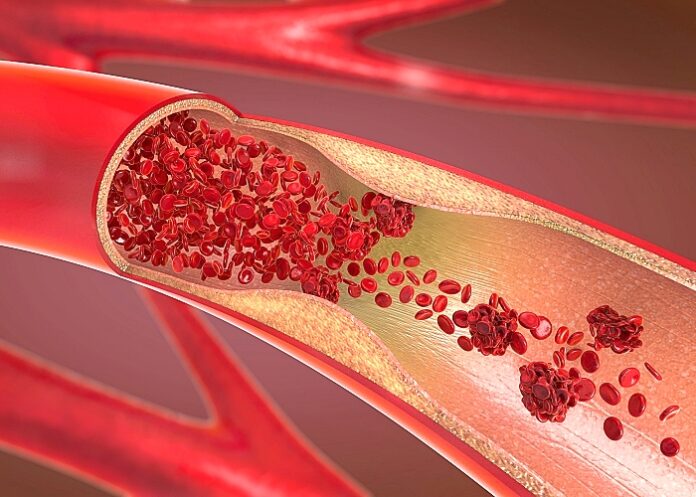
When the investigators looked at participants’ CTs, they found that, by the Coronary Artery Disease-Reporting and Data Systems (CAD-RAMS) scoring system, close to half (46%) had clear arteries with no signs of coronary artery disease. But that also meant that 54% had some blockage or stiffening of the arteries. The good news is that 27% of those people had minimal or mild coronary artery disease.
But a full 17% had confirmed obstructive coronary artery disease, and another one in 10 participants had the highest level of blockages. When they broke the data down by traditional and HIV-medication-related risk factors for coronary artery disease, they found something interesting. Although obesity was associated with the presence of atherosclerosis, it wasn’t associated with severe disease. But diabetes was the reverse of that: it wasn’t associated with the presence of the disease, but it was associated with more severe disease.
And when they looked at abacavir, they found no relationship between the drug and atherosclerosis. “Abacavir was not associated with the presence of atherosclerosis and was also not associated with severity of disease,” said Knudsen, in a Medscape Medical News report.
Although past use of AZT, indinavir, and didanosine were associated with severity of atherosclerosis, that association went away when Knudsen and team adjusted the findings for time since diagnosis. What was associated atherosclerosis was length of time living with HIV itself. For every five years a person lived with HIV, the study found the risk of having any atherosclerosis increased 20% and severity increased 23%. In addition, being a man was associated with a nearly 2.5-times increased risk of having any atherosclerosis and a 96% increased chance of having more severe atherosclerosis.
Having diabetes was associated with a nearly threefold increased risk of atherosclerosis, as was every additional decade of life for a person who was living with HIV.
The findings confirm the baseline data of the REPRIEVE trial, which recently released data showing similarly high rates of atherosclerotic plaque in people living with HIV who didn’t register as “at risk” for cardiovascular disease using traditional scoring methods.
“It’s important in that it’s a huge study that's confirmatory [of] what we know, which is that there are high levels of subclinical coronary artery disease in people living with HIV,” said Prof Steven Grinspoon from Harvard Medical School in Boston, Massachusetts, and principal investigator of REPRIEVE.
As for the lack of association between abacavir and cardiovascular risk, he said he would take the findings with a pinch of salt. “It’s hard to make a lot out of that,” he said. “It’s hard to know in a cross- sectional study. People put people on different things.”
In Spain, where Dr Jose Ignacio Bernardino treats people living with HIV at La Paz University Hospital in Madrid, abacavir is mostly a moot point, as clinicians have long since moved away from maintaining people living with HIV on any abacavir-containing regimens. What’s more important in the study, he told Medscape Medical News, is that “worrisome” high level of risk. REPRIEVE will test whether statins can reduce heart disease events in people living with HIV. But in the meantime, he said the take-away for clinicians from the study is the primary importance of traditional cardiovascular risk factors.
“We have to acknowledge that the major cardiovascular risk factor is age,” he said. “When patients are approaching their 50s, I usually try to stress a lot about cardiovascular risk factors in general. I stress healthy lifestyle — get physical exercise, hypertension, glucose, lipids — in every single patient.”
Study details
More than half of well-treated persons living with HIV have angiography verified coronary artery disease
A.D. Knudsen, A. Fuchs, T. Benfield, J.T. Kühl, P. Sigvardsen, L. Køber, S.D. Nielsen
Presented at the 18th European AIDS Conference (27-30 October 2021)
Purpose
Coronary artery disease (CAD) is common among persons living with HIV (PLWH). The pathogenesis likely includes traditional and HIV-specific factors including combination antiretroviral therapy (cART). We examined if cART would be associated with CAD in PLWH.
Included from The Copenhagen Co-morbidity in HIV Infection (COCOMO) Study: all participants of COCOMO were offered a high-resolution research coronary CT angiography, and we included all participants with a coronary CT angiography. Questionnaires were used to obtain data on lifestyle and a physical exam was performed. Data on cART were obtained through review of medical charts. Scans were analyzed and reported according to the Coronary Artery Disease Reporting and Data System (CAD-RADS). We used ordinal logistic regression adjusted for a prespecified model including age, sex, hypertension, diabetes, and smoking status to investigate if HIV-related factors were associated with CAD.
In the included 705 participants, mean age was 51 (standard deviation, SD: 11) years, 77 (11%) were women, and 669 (96%) had suppressed viral replication. Of all included, 379 (56%) had CAD-RADS ≥ 1 and 121 (17%) had CAD-RADS ≥3 (obstructive disease) (figure 1). In adjusted analyses, we found age, male sex, hypertension, diabetes, current smoking, dyslipidemia, duration of HIV infection, current use of protease inhibitors, and ever use of indinavir, zidovudine or didanosine to be associated with more severe CAD-RADS. However, current use of protease inhibitors, and ever use of indinavir, zidovudine or didanosine were not associated with CAD after adjusting for duration of HIV infection (p= .22, p=.69, p=.70, and p=.10, respectively).
Conclusions
More than half of PLWH had angiography-verified CAD and traditional risk factors and duration of HIV infection was associated with more severe CAD. No other HIV-specific factors were associated with more severe CAD after adjusting for duration of HIV infection.
Medscape article – More Than Half of People Living With HIV Have Coronary Plaque (Open access)
Presentation – 18th European AIDS Conference: 29 October 2021
See more from MedicalBrief archives:
Cardiovascular risk higher for people with HIV
Abacavir ART not increasing risk of myocardial infarction or CVD
Important to monitor kidney function in HIV patients doing well
Cardio-respiratory fitness and CVD mortality risk